Neurology:多发性硬化:不同临床分型,对应的灰质受累类型各有不同
2021-03-27 Freemann MedSci原创
Neurology:多发性硬化:不同临床分型,对应的灰质受累类型各有不同

在过去的几十年里,灰质(GM)受累越来越被认为是多发性硬化症(MS)病理生理学的一个重要组成部分。GM萎缩发生在MS的最早阶段,并随着时间的推移而进展,复发-缓解性MS(RRMS)患者的萎缩率是对照组的倍,而进展性MS患者的萎缩率则高达倍。
一直以来,GM萎缩与临床残疾之间存在实质性关系。GM萎缩的区域分布在各表型中并不均匀,深GM和顶叶较早受累,在疾病后期,GM损失逐渐扩散到额叶、颞叶、枕叶和小脑区域。
意大利Vita-Salute San Raffaele University的Maria A. Rocca等人,使用基于源的形态测量(SBM),探究了GM萎缩特点以及这种萎缩在不同MS表型中的1年演变情况。
他们从8个欧洲站中心,纳入170名健康对照组(HCs)和398名MS患者(34名临床孤立综合征[CIS],226名复发缓解MS[RRMS],95名继发性进展性MS[SPMS],43名原发性进展性MS[PPMS])中获得临床和MRI数据。57名HC和144名MS患者进行了1年的随访。并评估了基线GM损失、萎缩进展以及与残疾和1年临床恶化的相关性。
他们通过SBM确定了26个小脑、皮质下、感觉、运动和认知GM成分。
和HC相比,在MS中,GM萎缩几乎在所有成分中都有发现;CIS患者表现出环状的皮质下、小脑、颞部和显著性GM萎缩,而RRMS患者表现出广泛的GM萎缩。
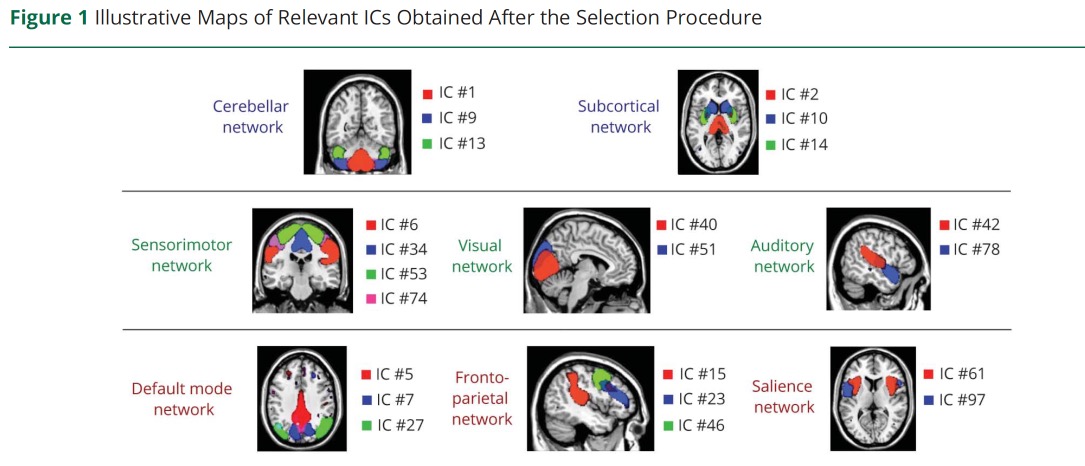
PPMS患者的小脑、皮层下、感觉运动、和额顶叶GM萎缩,SPMS与RRMS患者的GM萎缩。
1年时,21名(15%)患者临床病情恶化。MS中GM萎缩在皮质下、小脑、感觉运动和前颞顶叶成分中进展。基线较高的残疾与基线较低的正常化脑体积(β = -0.13,p = 0.001)、较大的感觉运动GM萎缩(β = -0.12,p = 0.002)和较长的病程(β = 0.09,p = 0.04)相关(R2 = 0.65)。
基线正常化GM体积(OR 0.98,p = 0.008)和小脑GM萎缩(OR0.40,p = 0.01)可独立预测临床恶化(曲线下面积0.83)。
这个研究的重要意义在于发现:GM萎缩在不同疾病表型中存在差异,并在MS后的一年中持续进展。除了全局性萎缩测量外,感觉运动和小脑的GM萎缩可以解释基线残疾和临床恶化。
原文出处:
Association of Gray Matter Atrophy Patterns With Clinical Phenotype and Progression in Multiple Sclerosis
Maria A. Rocca, Paola Valsasina, Alessandro Meani, et al.
Neurology Mar 2021, 96 (11) e1561-e1573; DOI: 10.1212/WNL.0000000000011494
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#多发性#
56
#Neurol#
52
学到了很多东西谢谢老师
102
学到了很多东西谢谢老师
90
学习了
106