Front Aging Neurosci:Lipocalin-2 在卒中后抑郁模型中调节海马小胶质细胞的激活
2021-12-21 brainnew神内神外 网络
海马体参与学习、记忆、情绪等基本功能,海马的病理改变是各种神经疾病的基础,特别是抑郁症、痴呆症和癫痫
卒中后抑郁症(PSD)是卒中后遗症之一,严重影响卒中幸存者的生活质量,并与高死亡率相关。其病理可能是多因素的,涉及中风和抑郁症的发病机制的组合,目前研究尚未阐明其发病机制,严重影响对PSD的预防和治疗。抑郁症被描述为一种与小胶质细胞相关的疾病,除了细胞过度活化和细胞数量增加外,在一些抑郁症患者中还观察到小胶质细胞数量减少和衰老,而小胶质细胞激活与PSD密切相关。
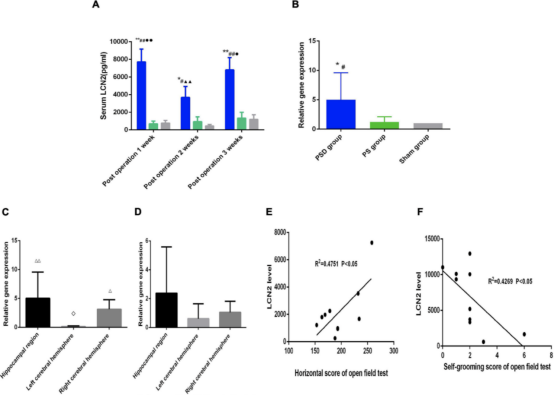
1、卒中后抑郁组1-3周LCN2浓度持续升高
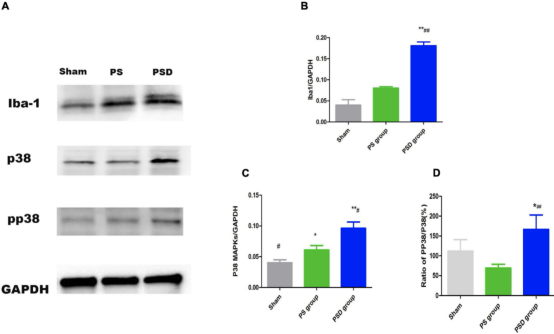
2、中风后抑郁大鼠海马区Iba1、P38 MAPK蛋白水平和 PP 38/P38 比值增加
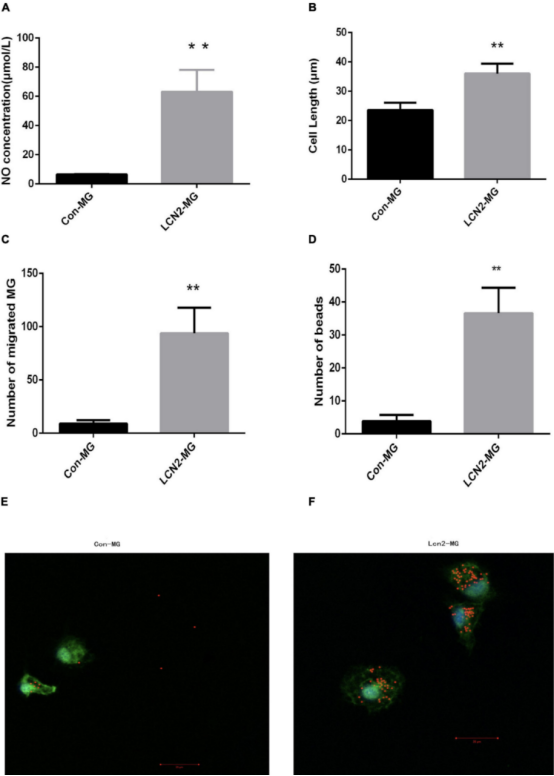
3、Lipocalin-2 刺激后小胶质细胞的变化
综上,作者研究发现LCN2可能通过P38/ MAPK 通路调节海马小胶质细胞的激活。
海马体参与学习、记忆、情绪等基本功能,海马的病理改变是各种神经疾病的基础,特别是抑郁症、痴呆症和癫痫。因此,研究海马小胶质细胞活化对于阐明PSD的机制具有重要意义。在之前的研究中,作者分析了PSD大鼠海马区、左右半脑小胶质细胞激活标志物的表达情况,发现海马比其他大脑区域有更多的小胶质细胞激活, PSD组大鼠海马区的小胶质细胞激活标志物 Iba1 的蛋白质水平显著增加。这表明海马的小胶质细胞在 PSD 中被激活,因此重点研究海马体。
在LCN2刺激后,初级小胶质细胞表现出明显的改变:小胶质细胞释放的NO量、小胶质细胞的长度、海马小胶质细胞的吞噬能力和迁移能力均显着增加。由于 P38 MAPK 和 LCN2 与小胶质细胞激活的密切关系,作者推测 LCN2可能通过P38/ MAPK 诱导小胶质细胞激活。因此,作者评估了 LCN2 刺激后海马小胶质细胞中 P38 MAPK 蛋白水平的变化,发现P38 MAPK 的相对蛋白水平显着增加。此外,PP38 MAPK蛋白水平也表现出同样显着的增加。P38 MAPK 和 PP38 MAPK 蛋白水平在PSD大鼠的海马中显示出与在培养的原代小胶质细胞中相同的变化。体外和体内结果均表明,LCN2通过在P38 MAPK途径调节海马小胶质细胞活化。
但是作者的研究存在局限性,作者研究的是整个海马区域,并没有区分不同的功能区域,所以需要进一步分析海马不同功能区域小胶质细胞激活的情况。
参考文献
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#卒中后#
66
#OCA#
54
#ROS#
56
#胶质细胞#
75
#IPO#
87
学习了,谢谢分享
72
好文章,谢谢分享。
70