ACEI和ARB不仅降压,还可能降低急性呼吸衰竭患者院内死亡率
2022-09-15 MedSci原创 MedSci原创 发表于上海
ACEI/ARB使用者成年 ARF 患者死亡率降低相关。未来,需要更高质量的随机对照试验来进一步证实以上结果。
呼吸衰竭是各种原因引起的肺通气和(或)换气功能严重障碍,以致不能进行有效的气体交换,导致缺氧伴(或不伴)二氧化碳潴留,从而引起一系列生理功能和代谢紊乱的临床综合征。而急性呼吸衰竭(ARF)继发于多种疾病,起病急骤、病情进展速度快,病死率高。据数据显示,在美国,ARF 的发病率为每 100,000 人中有 77.6-137.1 次住院,住院死亡率为 35.9%。
目前,针对ARF的急救治疗方法很多,体外膜肺以及各种呼吸支持技术等均在临床开展,使得急性呼吸衰竭患者的急救成功率显著上升。近年来,肾素-血管紧张素系统(RAS)对呼吸系统的调节作用,受到科研人员的广泛关注。
肾素-血管紧张素系统(RAS)是由一系列肽类激素及相应酶组成的重要的体液调节系统。主要功能是调节和维持人体血压、水、电解质的平衡,维持人体内环境的相对稳定。肾素-血管紧张素系统抑制剂(RASIs)广泛用于治疗高血压,主要包括血管紧张素转化酶抑制剂(ACEI)和血管紧张素受体拮抗剂(ARB)。几乎没有证据支持 ACEI 和 ARB 对呼吸衰竭患者的保护作用。
近日,发表在Pharmacotherapy杂志的一项回顾性观察研究,研究人员调查了 ARF 患者的死亡率是否因院前 ACEI 和 ARB 暴露而存在差异。

ACEI和ARB 类药物这个种类繁多,其中ACEI常用药有卡托普利、依那普利、赖诺普利及雷米普利等,而ARB常以「沙坦」命名,包括缬沙坦、氯沙坦、厄贝沙坦、替米沙坦、坎地沙坦、奥美沙坦和阿利沙坦。
其中,厄贝沙坦降压幅度较大,单药控制血压的达标率较高,吸收度高,药效持续时间长,在治疗高血压中占有重要地位。
在这项研究中,研究人员使用来自美国马萨诸塞州医疗中心大型公开数据库,该数据库名为Medical Information Mart for Intensive Care III v1.4 (MIMIC-III v1.4),记录了2001年至2019年期间贝斯以色列女狄肯斯医疗中心重症监护病房患者的相关数据,拥有4万多名患者的医疗健康数据和记录。
该研究最终纳入5335名成年ARF患者,包括363名ACEI/ARB使用者,总的院内死亡率为31.90%。与未使用ACEI/ARB患者相比,ACEI/ARB使用者年龄较大,急诊入院比例较低。在亚组分析中,除年轻患者外(<65 岁),所有亚组分析均支持 ACEI/ARB 对成年 ARF 患者的保护作用。对于年轻患者,ACEI/ARB 暴露不影响院内死亡率,而对于老年ARF 患者来说,ACEI/ARB的使用显著降低了院内死亡率。

使用ACEI/ARB与急性呼吸衰竭患者院内死亡率之间关系.
在经过倾向得分匹配(PSM)后,与非ACEI/ARB使用者相比,ACEI/ARB使用者院内死亡率(22.31% vs. 34.62%,p < 0.001)、28天死亡率(22.59% vs. 35.26%,p < 0.001)和90天死亡率(33.88% vs. 44.47%,p < 0.001)都明显降低,这与原始数据相同。
非ACEI/ARB使用者和ACEI/ARB使用者两组的住院时间相似,ACEI/ARB使用者为11.4天,非ACEI/ARB使用者为11.2天。与未使用ACEI/ARB的患者相比,使用ACEI/ARB的患者入院时的序贯器官衰竭估计评分(SOFA)和最大乳酸水平均有所下降。值得注意的是,在匹配队列中,急性肾损伤比例和住院期间通气比例没有发现明显的差异。
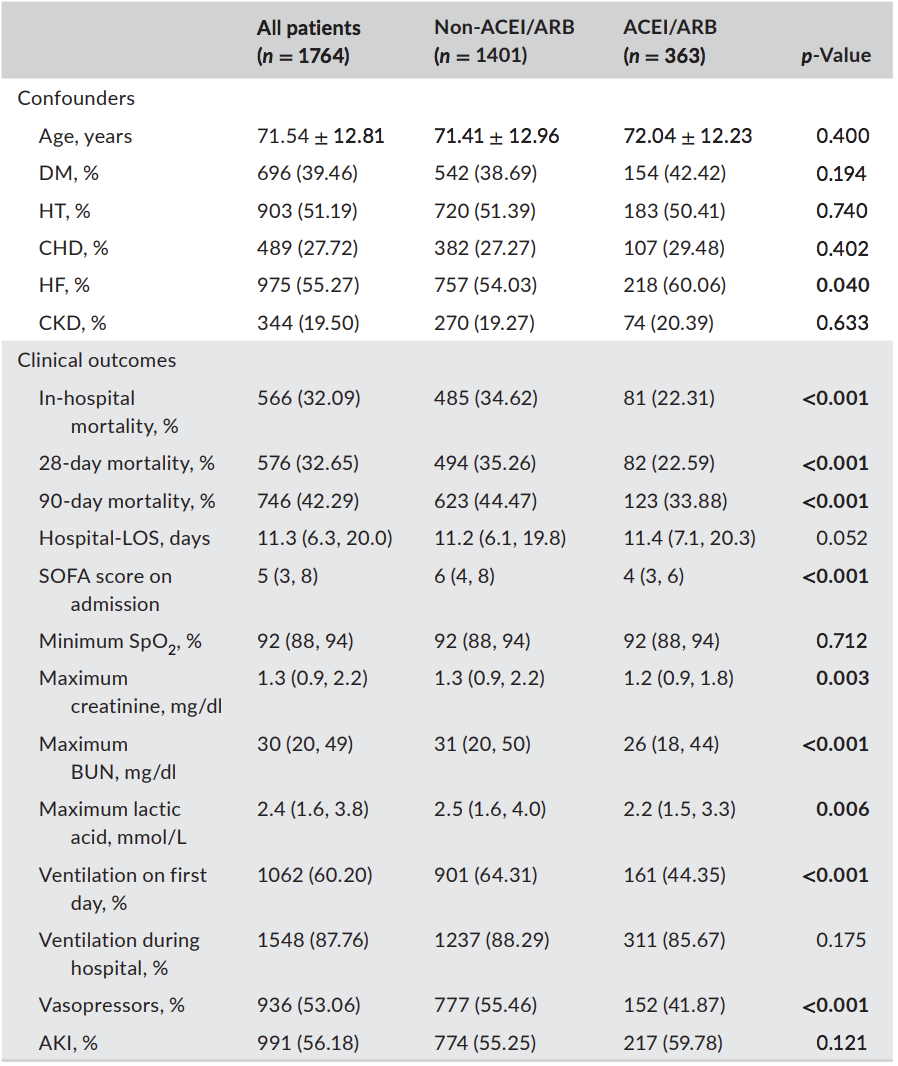
在ARF患者中,倾向得分匹配后的结果.
急性呼吸窘迫综合征(ARDS)是临床上常见的呼吸衰竭综合征。为了检验以上研究结果的准确性,研究人员从 MIMIC III 数据库进一步评估了 ACEI/ARB 对 ARDS 患者的疗效。总共从 MIMIC III 数据库中筛选出 4323 名 ARDS 患者,其中 449 名患者使用了 ACEI/ARB 。ACEI/ARB使用者在急性呼吸窘迫综合征(ARDS) 队列中表现出相似的效果,但在 MIMIC-IV 数据库中没有发现显著差异,这可能是由于 ACEI/ARB 使用者样本量好小。
MIMIC IV(1.0 版)是 MIMIC III 的更新数据库,包括 2008 年至 2019 年的重症监护数据库。MIMIC IV 数据库中有 5955 名 ARF 患者,其中 156 名患者有 ACEI/ARB 暴露。
总之,ACEI/ARB使用者成年 ARF 患者死亡率降低相关。未来,需要更高质量的随机对照试验来进一步证实以上结果。
原始出处
Fang YP, Zhang X. A propensity score-matching analysis of angiotensin-converting enzyme inhibitor and angiotensin receptor blocker exposure on in-hospital mortality in patients with acute respiratory failure. Pharmacotherapy. 2022 May;42(5):387-396. doi: 10.1002/phar.2677. Epub 2022 Apr 8. PMID: 35344607; PMCID: PMC9322533.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#院内死亡#
80
#ACE#
82
认真学习了
59
#降压#
82
#急性呼吸衰竭#
60
学习了
54