Eur Heart J:与健康人相比,心血管疾病患者从运动中获益更多
2019-09-17 佚名 中国生物技术网
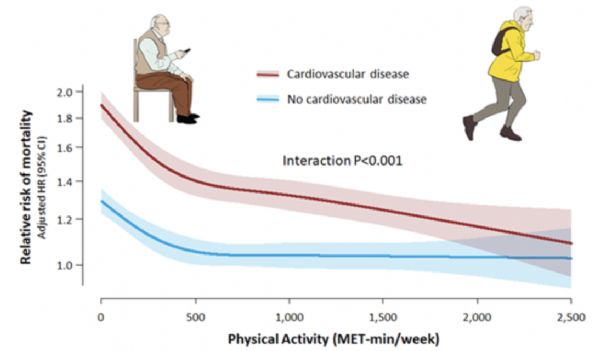
一项涉及大约50万人的研究首次发现,与没有心血管疾病(CVD)的健康人相比,有心脏或血管问题的人从积极的体育生活方式中获益更多。在对CVD患者及非CVD患者进行为期6年的追踪研究中,研究人员发现,增加体育运动能降低死亡风险,但是,死亡风险降低最明显的是CVD患者,如果他们加大运动量,则风险还会进一步降低。这项近日发表在《European Heart Journal》上的研究同时也在法国巴黎举行的欧
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#健康人#
53
#疾病患者#
45
#ART#
39
#血管疾病#
59
#HEART#
43
学习了,学习了
87