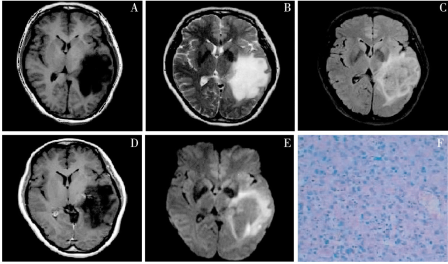
磁共振弥散张量纤维束成像技术在听神经瘤中的应用
2019-08-14 宋海民 吴至武 胡坤 中国现代医学杂志
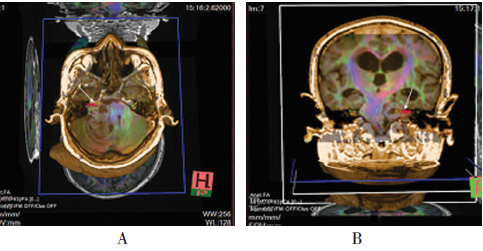
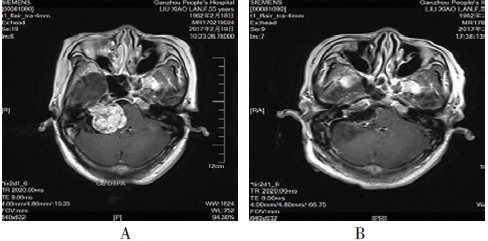
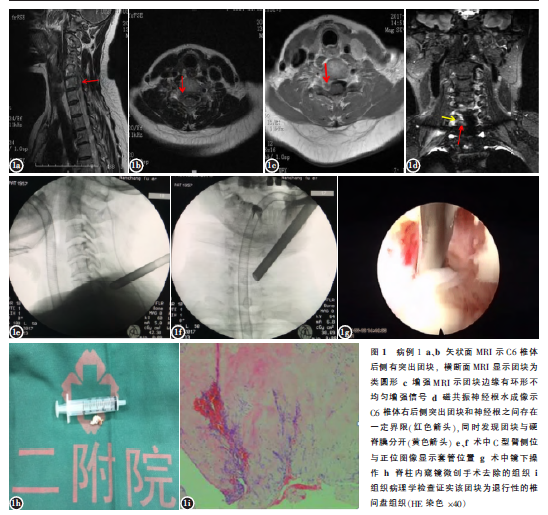
选取2016年1月-2017年2月于南昌大学附属赣州医院就诊的听神经瘤11例患者。其中,男性4例,女性7例;年龄38~68岁,平均(44.5±8.4)岁;病程2个月~20年。所有患者均有听力下降,其中听力丧失2例,4例术前面瘫明显。术前行头颅MRI平扫及增强扫描,运用DTI技术进行面神经成像检查。采用德国Siemens公司的3.0T磁共振机采集信号,参数为:重复时间6500ms,恢复时间95ms,

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#纤维束成像#
48
#神经瘤#
83
#磁共振#
36
#成像技术#
68
#听神经瘤#
59