BJH:达雷妥尤单抗、来那度胺和地塞米松在新诊断的与多发性骨髓瘤相关的全身性轻链淀粉样变性患者中的应用
2022-05-10 网络 网络
对于新诊断的与 MM 相关的全身性 AL 淀粉样变性患者,DRd 方案可能是一种有效的治疗选择,这些患者通常被排除在临床试验之外

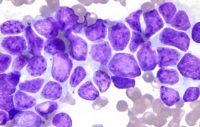
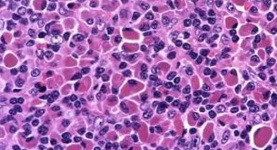
大约12%–15%的多发性骨髓瘤 (MM) 患者在临床过程中发展为全身性轻链淀粉样变性 (AL 淀粉样变性)。对 MM 相关的全身性 AL 淀粉样变性患者的需要探索更适合的治疗方案。在本回顾性队列研究中,研究人员分析了 达雷妥尤单抗、来那度胺和地塞米松 (DRd) 的 6 个月血液学和器官反应,DRd 是新诊断的移植不合格 MM 患者的护理标准,其中3名 MM 患者在诊断时伴有全身性 AL 淀粉样变性。
根据国际骨髓瘤工作组 (IMWG) 标准,数据收集诊断为患有 MM和全身性 AL 淀粉样变性,从2019 年 11 月至-2021 年 4 月在熊本大学医院接受治疗的患者。共有 10 名新诊断的患者入组,预先接受 DRd 方案治疗。由于年龄或器官功能障碍,所有患者都被认为不适合进行自体干细胞移植。该研究一半的患者年龄超过 75 岁,80% 的患者处于 Mayo 2012 AL 淀粉样变性分期系统的 3 或 4 期。没有患者是 Mayo 2004 3B 期,这被认为是预后特别差的亚组,中位生存期为 3 个月。
根据 AL 淀粉样变性的器官受累标准,10 名患者中有 9 名患有心脏淀粉样变性。3例患者患有肾淀粉样变性,其中1例患有肾病综合征。所有患者最初接受静脉注射达雷妥尤单抗(16 mg/kg/周),在日本获批后转为皮下注射达雷妥尤单抗(1800 mg/周)。来那度胺从第 1-21 天开始口服,每 28 天重复一次。没有患者每天接受超过15mg的来那度胺,由每位医生根据肾功能和一般情况进行调整。考虑到高龄或心力衰竭,所有患者每周给予地塞米松 20 mg。

图1:新诊断的多发性骨髓瘤 (MM) 系统性 AL 淀粉样变性患者对达雷妥尤单抗、来那度胺和地塞米松 (DRd) 的治疗反应。(A) 根据国际骨髓瘤工作组 (IMWG) 统一反应标准,在 DRd 治疗后 6 个月时的血液学反应。(B) 根据 AL 淀粉样变性血液学反应标准,在 DRd 治疗后 6 个月时的血液学反应。由于基线时 dFLC <50 mg/l,一名患者被排除在分析之外。(C) 有(左)或无(右)心脏反应的患者 DRd 治疗 6 个月后 BNP 水平的变化。(D) 接受 DRd 治疗的患者的 Kaplan-Meier 总生存期。sCR,严格的完全反应;CR,完全响应;VGPR,非常好的部分响应;PR,部分响应;SD,疾病稳定;NR,没有回应;法国巴黎银行
在数据截止日期(2021 年 12 月 1 日),中位随访时间为 11.5 个月后,患者接受了中位 8.5 个周期的 DRd 治疗。根据 IMWG 统一反应标准(图 1A)和 AL 淀粉样变性血液学反应标准(图 1B),DRd 治疗后 6 个月的总体血液学反应为 90% 和 88.9%。超过 50% 的患者实现了非常好的部分反应 (VGPR) 或更好的血液学反应,这与系统性 AL 淀粉样变性患者的生存率显着提高有关。
已知 t(11;14) 易位的存在与 AL 淀粉样变性患者对硼替佐米的低敏感性有关。在 t(11;14) 阳性和阴性病例之间未观察到 DRd 治疗对血液学反应的显着差异。在 DRd 治疗后 6 个月,在没有血液学反应的单个患者中检测到染色体 1q21 扩增。由于 10 名患者中有 9 名患有 AL 淀粉样变性的心脏受累,因此在治疗后 6 个月评估心脏反应。由于熊本大学医院对 N 端脑利钠肽前体 (NT-proBNP) 的访问有限,因此使用脑利钠肽 (BNP) 来分析心脏反应。8 名患者的基线 BNP ≥150 pg/ml,并根据最近建立的基于 BNP 的评估心脏对 AL 淀粉样变性治疗反应的标准进行心脏反应分析。尽管之前的一项研究报告了来那度胺治疗的 AL 淀粉样变性患者的 BNP 升高,但8 名患者中有12名(50%)实现了心脏反应(图 1C)(≥50 pg/ml 和 ≥30% 的 BNP 降低)。在 3 例肾淀粉样变性患者中,2 例无肾病综合征患者实现了肾脏反应,而肾病综合征患者的反应稳定。在数据截止时,10 名患者中有 8 名仍在接受 DRd 治疗,9 名患者在没有疾病进展的情况下存活。一名患者在治疗开始后 15 个月时因肠道淀粉样变性而死于肠穿孔。24 个月时的估计总生存率为 80%(图 1D)。在 DRd 治疗期间未观察到 4 级不良事件。中性粒细胞减少症是最常见的 3 级不良事件,并未导致治疗中断。一名患者在两个周期的 DRd 后因 3 级肠梗阻而停止治疗。然而,根据 IMWG 反应标准,患者在治疗开始 24 个月后实现了严格的完全反应 (sCR),没有任何疾病进展迹象。
合并 MM 的系统性 AL 淀粉样变性患者通常被排除在系统性 AL 淀粉样变性和 MM 3 期试验之外。由于 12%–15% 的 MM 患者发生全身性 AL 淀粉样变性,因此需要对这些患者进行适当的治疗方案。目前的研究表明,在治疗开始后 6 个月,DRd 会引起高度的血液学和心脏反应。尽管队列中的患者年龄相对较大并且患有晚期淀粉样变性,但大多数人能够继续 DRd,毒性有限。值得注意的是,在该队列中,来那度胺的剂量减少到中位数 10 mg/天。减少来那度胺的剂量可能是继续治疗的一个重要因素,因为全身性 AL 淀粉样变性患者通常不能耐受超过 15 毫克/天的来那度胺。一名在 DRd 治疗后 6 个月没有血液学反应的患者出现染色体 1q21 扩增。先前发表的一篇报道 DRd 方案对复发或难治性系统性 AL 淀粉样变性患者的疗效的出版物表明,1q21 扩增的存在可能会降低 DRd 的疗效。尽管治疗反应低的确切机制尚不清楚,但 1q21 扩增的患者可能需要考虑 DRd 以外的方案。
总之,对于新诊断的与 MM 相关的全身性 AL 淀粉样变性患者,DRd 方案可能是一种有效的治疗选择,这些患者通常被排除在临床试验之外。由于目前的研究是来自单个机构的少数患者队列,因此需要多个机构进行更长随访时间的前瞻性研究进行验证。
原始出处:
Kawano, Y., Hata, H., Takashio, S., Tsujita, K., Ueda, M. and Matsuoka, M. (2022), Daratumumab, lenalidomide and dexamethasone in newly diagnosed systemic light chain amyloidosis patients associated with multiple myeloma. Br J Haematol. https://doi.org/10.1111/bjh.18234
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#新诊断#
87
#多发性#
75
#轻链淀粉样变性#
64
#淀粉样变#
82
#淀粉样变性#
77
#变性#
60
有用,学习了
94