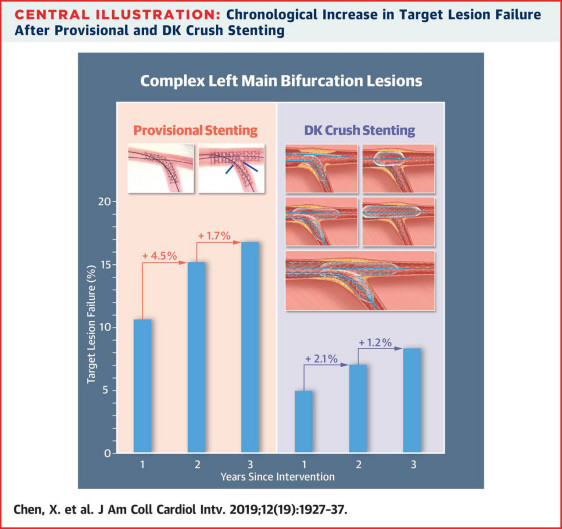
JACC Cardiovasc Interv:陈绍良团队分叉病变处理3年随访结果:治疗无保护左主干分叉病变,DK Crush技术完胜单支架技术
2019-10-22 卢芳 中国循环杂志
10月14日,JACC子刊刊发南京市第一人民医院陈绍良团队DKCRUSH-V试验3年随访结果,结果显示,对于无保护左主干分叉病变,DK Crush技术完胜单支架技术。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#随访结果#
54
#ASC#
59
#左主干#
66
#JACC#
45
#ACC#
45
#分叉病变#
63
写得好
81