Gastroenterology Report:急诊手术后转入ICU的急性小肠穿孔患者死亡率的预测因素
2022-08-19 xuyihan MedSci原创
若为小肠穿孔,面积比较小,腹腔污染相对较轻,及时进行手术修补破裂的肠管,并清理腹腔内的液体,放置引流管,一般不会影响患者的生命。
胃肠道 (GI) 穿孔是一种常见的外科急症,具有很高的发病率和死亡率,最初,患者常出现突然腹痛,严重患者可出现继发于腹膜炎的感染性休克症状。与整个胃肠道其他部位的穿孔相比,小肠穿孔并不常见,并且通常表现出非典型的临床表现。然而,小肠穿孔更容易发生严重甚至危及生命的感染。机械性梗阻和免疫介导疾病(克罗恩病)是西方国家的小肠穿孔的主要原因,而继发于伤寒和肺结核的小肠穿孔在发展中国家更为常见。本研究回顾性分析了接受小肠穿孔急诊手术的ICU 患者,旨在探究术后死亡率相关的预后因素。
研究人员回顾性分析2011年2月至2020年5月间经急诊手并转入复旦大学中山医院ICU治疗的小肠穿孔患者的临床数据。将患者的医疗记录进行详细分析以确定临床特征、实验室指标、手术结果和病理学的差异。

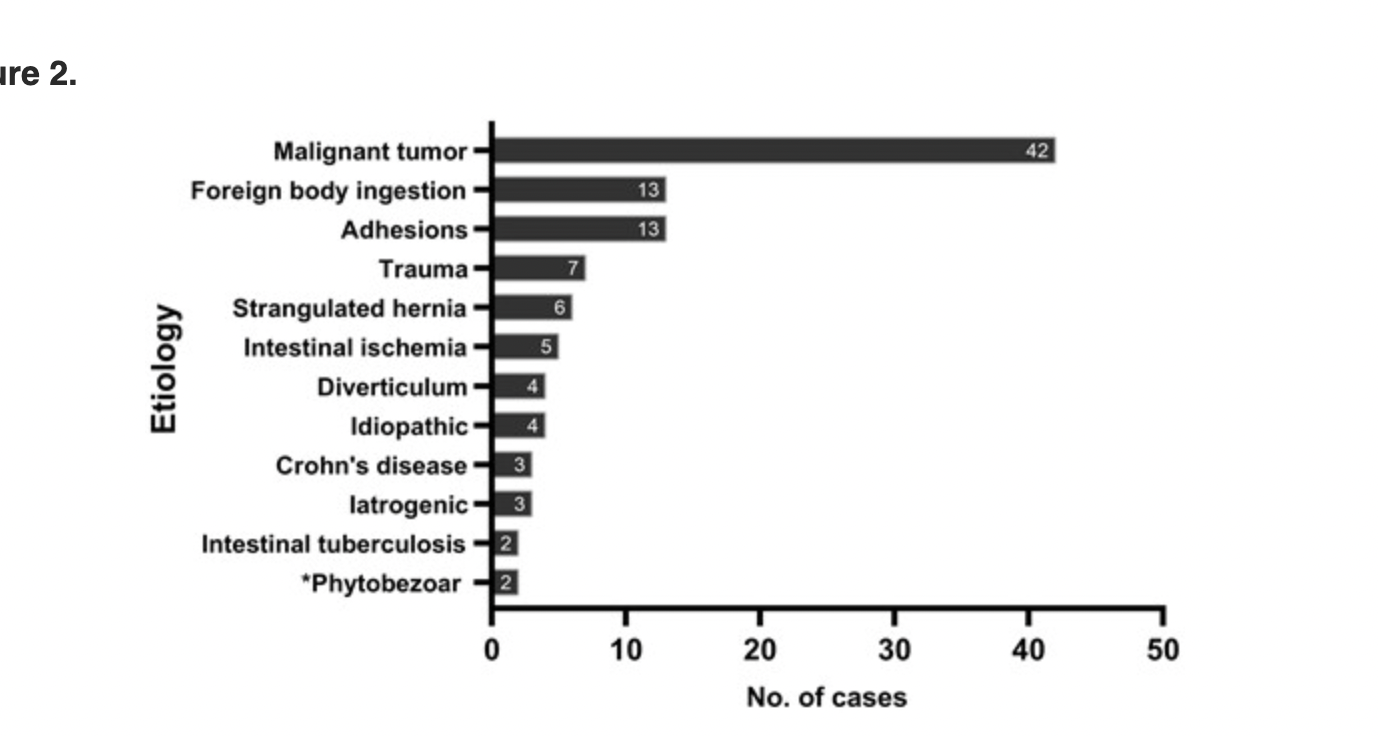
本研究共纳入104例患者,其中18例(17.3%)接受了穿孔修复、59例(56.7%)接受了肠段节段切除一期吻合和27例(26.0%)接受了小肠造口术。恶性肿瘤是这些患者穿孔的主要原因(40.4%,42/104)。总体术后并发症发生率和死亡率分别为 74.0% (77/104) 和 19.2% (20/104)。恶性肿瘤相关穿孔(优势比 [OR],4.659;95% 置信区间 [CI],1.269-17.105;P = 0.020)和高术后动脉血乳酸水平(OR,1.479;95% CI,1.027 –2.131;P=0.036)被确定为转移到ICU的小肠穿孔患者术后死亡率的独立危险因素。
本项研究证实急诊手术后转入ICU的小肠穿孔患者面临术后并发症和死亡的高风险。此外,恶性肿瘤相关穿孔和术后血乳酸水平较高的患者预后较差。
原始出处:
Jianzhang Wu. et al. Predictors of mortality in patients with acute small-bowel perforation transferred to ICU after emergency surgery: a single-centre retrospective cohort study.Gastroenterology Report.2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














#Gastroenterol#
0
#患者死亡#
84
#GAS#
78
#AST#
67
#预测因素#
79
#穿孔#
79
#Gastroenterology#
0
#急诊手术#
66
#肠穿孔#
69