Cell:邓宏魁组报道新型多能干细胞系
2017-04-10 李华芸 Bioart
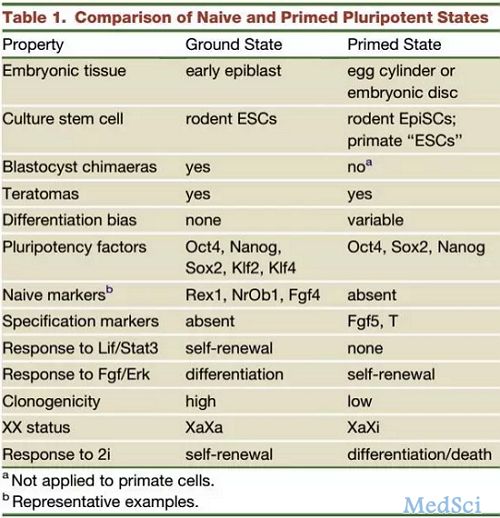
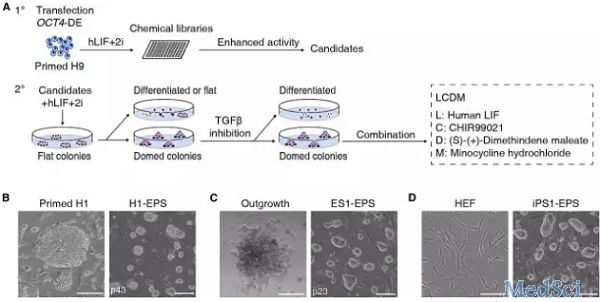
4月6日,Cell杂志发表了来自北京大学邓宏魁教授课题组题为“Derivation of Pluripotent Stem Cells with In Vivo Embryonic and Extraembryonic Potency”的最新重要研究成果,该研究系首次在国际上建立了具有全能性特征的多潜能干细胞系(EPS细胞),获得的细胞同时具有胚内和胚外组织发育潜能,并且该研究中还证明了人EP


本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#干细胞系#
52
#Cell#
45
#CEL#
33
#细胞系#
41
文章不错,值得分享
68