Acta Radiol: 前列腺肿瘤放射治疗后的监测研究
2018-09-26 AlexYang MedSci原创
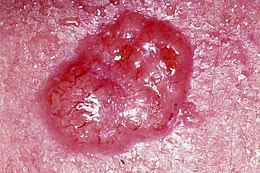
放射治疗后效果的纵向监测可以通过动态超声造影成像(DCE-US)来实现。最近,有研究人员利用DCE-US在一个人类前列腺癌小鼠皮下模型中评估了相关的功能性参数,并且探究了治疗后剂量累计和时间时限的相关性。另外,研究人员还特别关注且评估了肿瘤的血管异质性,并利用了最合适的数据分析方法来反应上述异质性。研究人员在 7.5 Gy和10 Gy单独剂量放射治疗后的24小时和48小时时分别获得了DCE-US数
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#前列腺肿瘤#
67
#CTA#
64
#肿瘤放射治疗#
48
学习了谢谢分享
92
学习了,谢谢分享。
88