Nat Med:清除衰老细胞使关节重焕青春
2017-05-09 佚名 药明康德
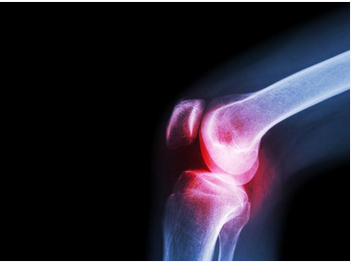
骨关节炎(osteoarthritis)是一种困扰着许多中老年人的疾病,它是由于关节中软骨由于运动或其它原因造成损伤后出现退化,导致关节内出现骨质增生而形成慢性炎症。该病的主要症状是关节疼痛和肿胀,严重影响日常生活。▲健康的关节中(左),软骨覆盖骨头的末端,充当垫子或减震器,并且在骨骼之间提供光滑的表面。在骨关节炎中(右),软骨发生损伤,骨头会相互摩擦,随着时间的推移,这种摩擦会永久损坏关节。(图
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#Nat#
78
有点意思
97
新角度看问题,值得学习!
84
学习了
105
学习了,谢谢作者分享!
77
学习了,科研终究有天用于临床
89
学习了,谢谢作者分享!
53
学习了谢谢了。
55
#Med#
50
好东西学习了!
55