Nat Med:T细胞受体疗法(TCR)治疗骨髓瘤疗效良好
2016-05-06 MedSci MedSci原创
1/2期试验结果显示,对于多发性骨髓瘤患者,自体干细胞移植之后进行新型T细胞受体(TCR)疗法治疗是安全的,而且与临床缓解和无进展生存期改善相关。 Aaron Rapoport及其同事写到,骨髓瘤的自体免疫调节是可能发生的,因为存在于骨髓瘤患者血液和骨髓瘤中的肿瘤活化T细胞可靶向骨髓瘤细胞。研究者还写道,对于黑素瘤的早期临床试验、研究者推荐TCR设计的T细胞,但是其临床结果差强人意。
1/2期试验结果显示,对于多发性骨髓瘤患者,自体干细胞移植之后进行新型T细胞受体(TCR)疗法治疗是安全的,而且与临床缓解和无进展生存期改善相关。文章发表在Nature Medicine上,Lancet Oncology配发了评论。
Aaron Rapoport及其同事写到,骨髓瘤的自体免疫调节是可能发生的,因为存在于骨髓瘤患者血液和骨髓瘤中的肿瘤活化T细胞可靶向骨髓瘤细胞。研究者还写道,对于黑素瘤的早期临床试验、研究者推荐TCR设计的T细胞,但是其临床结果差强人意。
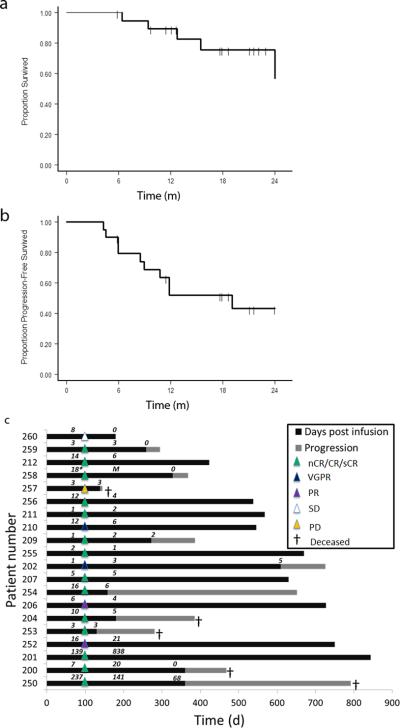
Rapoport及其同事评估了自体T细胞设计表达亲和力增强的TCR的安全性和有效性,它可以识别肿瘤-睾丸抗体NYESO-1和LAGE-1共享的缩氨酸。大约60%的晚期骨髓瘤患者表达NY-ESO-1。20名显示抗体阳性的多发性骨髓瘤患者接受自体干细胞移植2天后,接受平均2.4 × 10⁹的工程T细胞输注。T细胞输注耐受性良好,尽管白介素6浓度较高,但是没有出现明显的临床细胞因子释放综合征。
治疗之后中位随访21.1个月(95% CI 12.7–22.9)10/20名患者仍然无进展生存,15名患者存活,5名死亡。治疗后的100天,14名患者发生接近完全缓解或完全缓解。中位无进展生存期为19.1个月(95% CI 8.5–未达到)的16名患者发生良好的临床缓解。
Carl June说,这是第一项显示表达高亲和力TCR的基因修饰T细胞有长期表达和功能的研究。这些细胞存在于大多数患者中,而且似乎对缺乏不良反应的患者具有长期抗肿瘤活性。多发性骨髓瘤通常是不可治愈的,因此,这一研究结果是良好的,因为williamhill asia 观察到良好的临床缓解。然而,这一疗法用于临床实践之前需要进行更大型的研究。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#Nat#
37
学习了,很好的
139
学习了,很好的
147
#TCR#
51
#T细胞受体#
0
#Med#
35
希望之光
114