单纯血栓切除术是否与静滴阿替普酶联合血栓切除术同样有效仍存在争议。该研究旨在确定在急性缺血性卒中患者中单纯取栓是否不劣于静滴阿替普酶+取栓。
这是一项多中心、随机、开放标签、预后盲法的临床试验,招募了因大血管闭塞而在血管中心接受 CT 或磁共振血管造影证实的卒中患者,随机(1:1)分成两组,接受单纯取栓或静滴阿替普酶+取栓术。主要终点是第90天时改良的Rankin量表得分≤2分。
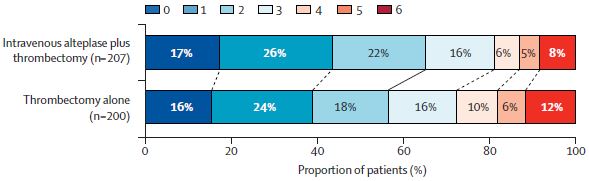
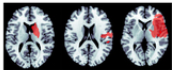
两组第90天时改良的Rankin量表得分
2017年11月29日至2021年5月7日期间,共筛查了5215位患者,其中423位被随机分组,最终408位(201位接受单纯取栓,207位接受静滴阿替普酶+取栓)被纳入主要疗效分析。单纯取栓术组和阿替普酶+取栓术组分别有115位(57%)和135位(65%)在第90天时改良的Rankin量表得分≤2分(校正的风险差 -7.3%,95% CI -16.6~2.1;单侧95% CI的下限是-15.1%,超过了-12%的非劣效性界限)。
两组的安全性结局
仅接受血栓切除术的201位患者中有6位 (2%) 、接受静滴阿替普酶联合血栓切除术的202位患者中有7位 (3%) 出现了症状性颅内出血(风险差 -1.0%,95% CI -4.8~2.7)。仅接受血栓切除术的患者的再灌注成功率较低(91% vs 96%,风险差 -5.1%,95% CI -10.2~0.0,p=0.047)。
综上,该研究未能证实单用血栓切除术不劣于静滴阿替普酶联合血栓切除术,单用血栓切除术会导致再灌注率降低。该结果不支持符合条件的患者在取栓前省略静滴阿替普酶。
原始出处:
Urs Fischer, et al. Thrombectomy alone versus intravenous alteplase plus thrombectomy in patients with stroke: an open-label, blinded-outcome, randomised non-inferiority trial. The Lancet. July 09, 2022. https://doi.org/10.1016/S0140-6736(22)00537-2
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#Lancet#
95
#卒中患者#
79
#取栓#
98
lancet上果然牛,感谢williamhill asia 更新及时
82