JAHA:功能性二尖瓣关闭不全的严重程度可预测心衰患者再住院和死亡的长期风险
2021-12-24 MedSci原创 MedSci原创
超过一半因急性失代偿性心力衰竭和左心室收缩功能障碍住院的患者至少存在中度功能性二尖瓣关闭不全,这与患者再入院率和死亡率增加相关。
功能性二尖瓣关闭不全已成为慢性心力衰竭和左心室收缩功能障碍患者的治疗靶标。功能性二尖瓣关闭不全在急性失代偿性心力衰竭患者中的意义仍不明确。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在这项研究中,研究人员系统地调查了急性失代偿性心力衰竭和左心室收缩功能障碍患者入院时功能性二尖瓣关闭不全的患病率和临床意义。

该研究是对2012年至2017年期间因急性失代偿性心力衰竭和左心室收缩功能障碍入院的患者进行的单中心回顾性研究。根据功能性二尖瓣关闭不全的严重程度,患者被分为3组:无/轻度、中度和中度至重度/严重的功能性二尖瓣关闭不全。该研究的主要结局是患者出院后1年的全因死亡率。研究人员还比较了这些组别6个月的心力衰竭住院率。
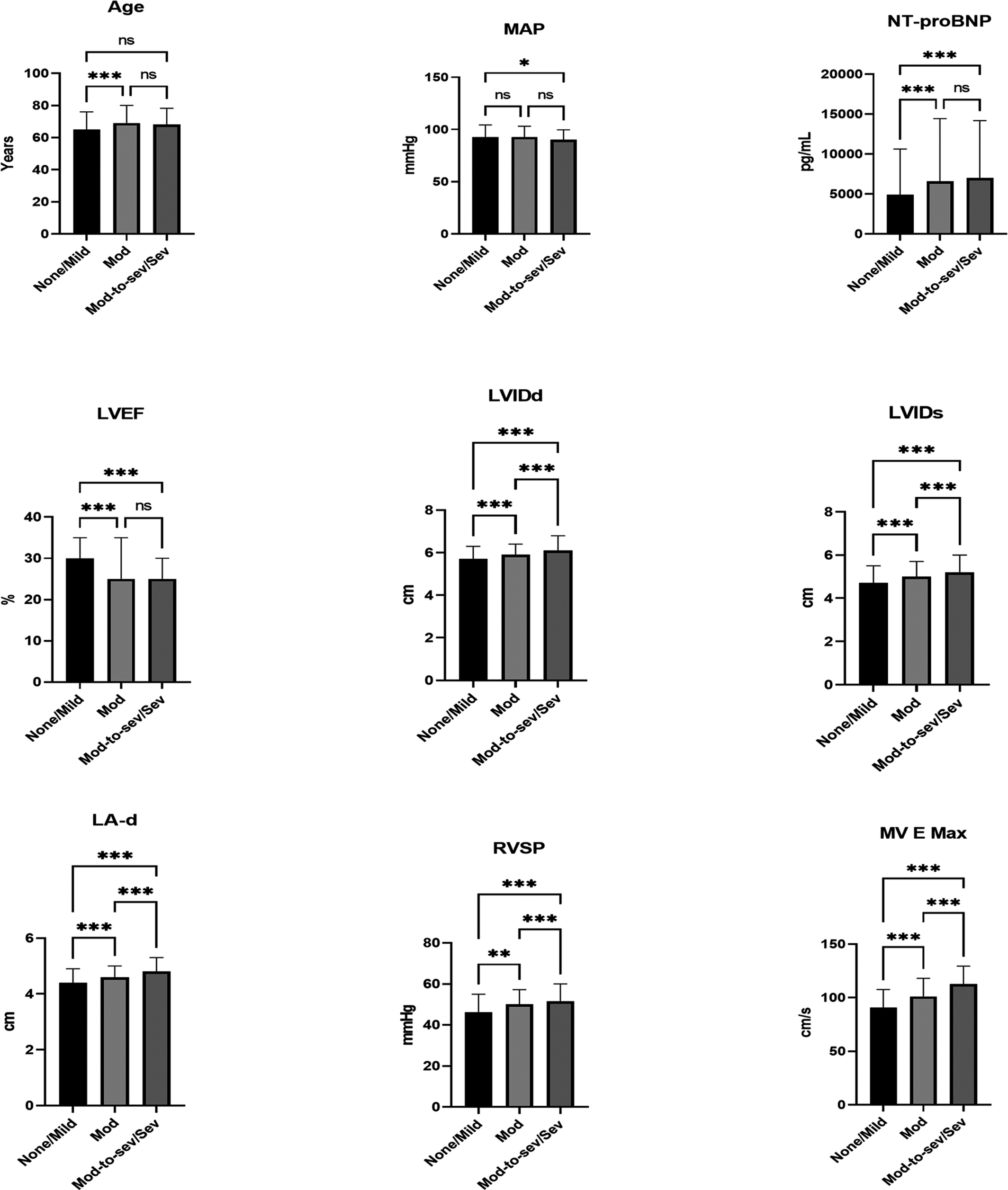
在2303名患者中,39%(896人)的患者为女性。左心室射血分数中位数为25%。453名(20%)患者出现了中度至重度/重度功能性二尖瓣关闭不全,这与患者1年全因死亡率独立相关。在1210名(53%)患者中发现了中等或严重程度更差的功能性二尖瓣关闭不全,并且与6个月的心力衰竭住院独立相关。女性与较高的功能性二尖瓣关闭不全严重程度独立相关。
由此可见,超过一半因急性失代偿性心力衰竭和左心室收缩功能障碍住院的患者至少存在中度功能性二尖瓣关闭不全,这与患者再入院率和死亡率增加相关。应加强出院后随访,以消除适合药物治疗的功能性二尖瓣关闭不全,并对持续性功能性二尖瓣关闭不全进行及时和适当的干预。需要进一步的研究来评估功能性二尖瓣关闭不全的性别差异。
原始出处:
Rachna Kataria,et al.Severity of Functional Mitral Regurgitation on Admission for Acute Decompensated Heart Failure Predicts Long‐Term Risk of Rehospitalization and Death.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.022908
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#功能性#
58
#二尖瓣关闭不全#
60
#AHA#
60
#心衰患者#
105
#长期风险#
60
#二尖瓣#
70
学习了
83