Eur Heart J:无症状脑梗死对心房颤动患者认知功能的影响
2022-02-18 MedSci原创 MedSci原创
在当代AF患者队列中,5.5%的MRI检查个体显示2年后出现新的脑梗死。这些梗塞个体大多数在临床上是无症状的,并且发生于抗凝患者中。临床上,明显和无症状的脑梗塞对认知能力下降存在类似的影响。
心房颤动(AF)是死亡、卒中、心力衰竭、认知功能障碍和痴呆的重要危险因素。研究人员之前报道了一项横断面分析的数据,其中大约五分之一的AF患者在系统性脑磁共振成像(MRI)检查图像上存在临床上无症状的脑梗塞。无症状脑梗塞与认知功能障碍之间的关联与临床卒中的关联相似,因此这一结果为既往无卒中个体AF与认知能力下降之间的关联提供了潜在的解释。AF患者微出血(Mb)和白质病变(WML)负担也很重。
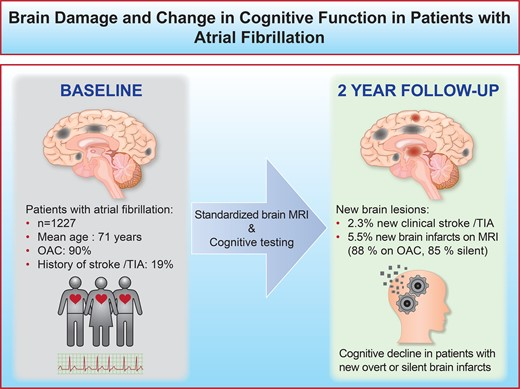
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在探究临床上明显和无症状的脑损伤与心房颤动(AF)患者认知功能之间的关联。

研究人员在一项前瞻性、多中心队列研究(Swiss-AF)中招募了1227名AF患者。患者在基线和2年后接受了标准化的脑磁共振成像(MRI)检查。研究人员量化了新的小型非皮质梗死(SNCI)和大型非皮质或皮质梗死(LNCCI)、白质病变(WML)和微出血(Mb)病灶。临床上,无症状性梗死被定义为随访期间未发生临床卒中或短暂性脑缺血发作(TIA)的患者在随访MRI上出现了新的SNCI/LNCCI。研究人员使用经过验证的测试评估了受试者的认知功能。
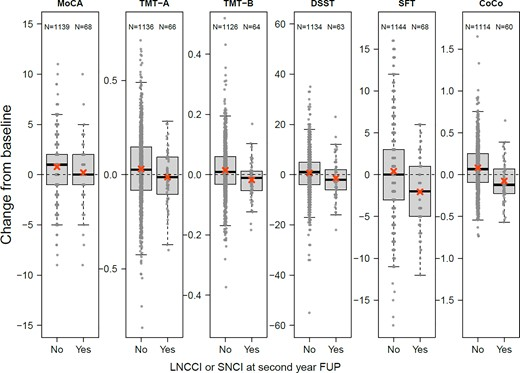
受试者平均年龄为71岁,26.1%为女性,89.9%接受抗凝治疗。在2年的随访期间,28名患者(2.3%)经历了卒中/TIA。在SNCI/LNCCI≥1的68名(5.5%)患者中,60名(88.2%)患者在基线时进行了抗凝治疗,58名(85.3%)患者伴有无症状梗死。与没有新发脑梗塞的患者[0.07(-0.09,0.25)]相比,脑梗死患者的认知结构评分[-0.12(-0.22,-0.07)]变化更大。新的WML或Mb与认知能力下降无关。
由此可见,在当代AF患者队列中,5.5%的MRI检查个体显示2年后出现新的脑梗死。这些梗塞个体大多数在临床上是无症状的,并且发生于抗凝患者中。临床上,明显和无症状的脑梗塞对认知能力下降存在类似的影响。
原始出处:
Michael Kühne,et al.Silent brain infarcts impact on cognitive function in atrial fibrillation.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac020/6529516
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#无症状脑梗死#
63
#ART#
68
#脑梗#
73
#无症状#
66
#HEART#
55
#心房#
54
#心房颤动##认知功能#
120