Lancet Oncol:Pembrolizumab获批一线联合化疗治疗晚期NSCLC(KEYNOTE-021)
2017-05-20 佚名 肿瘤前沿
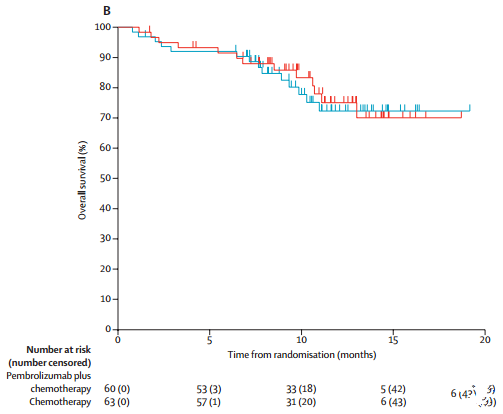
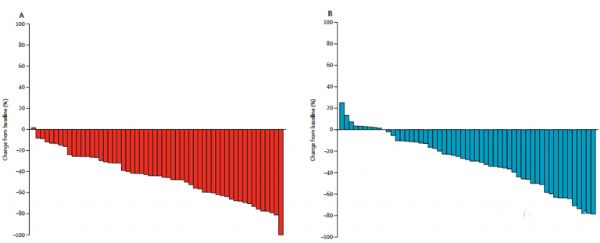
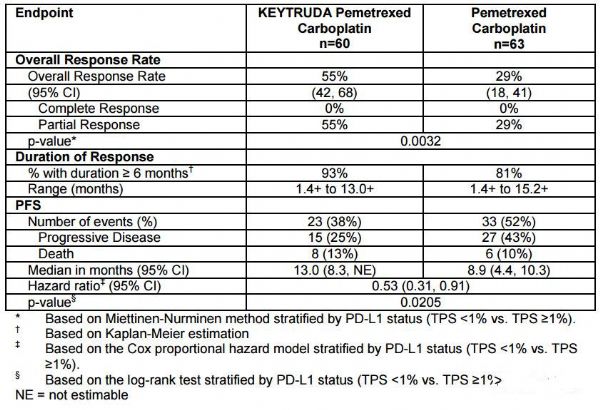
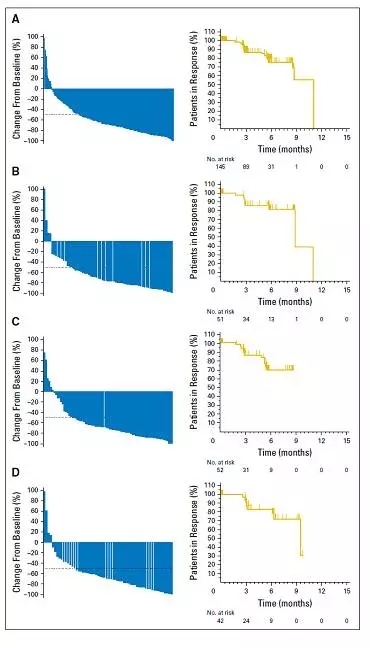
2017年5月10日,美国FDA加速批准了Pembrolizumab(Keytruda)联合培美曲塞+卡铂用于既往未经治疗的无突变的晚期NSCLC患者(非鳞癌)的治疗。这项适应症的获批使得Keytruda的说明书再次更新(之前的一次是2017年02月份的更新),而且把免疫单抗对于肺癌的治疗带入了一个新阶段,即联合化疗的全新治疗模式。该适应症的批准是基于一项名为KEYNOTE-021的多中心、开放、
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#Lancet#
45
#Oncol#
59
#KEYNOTE#
55
#mAb#
40
#Pembro#
59
#PE#
52
#Pembrolizumab#
59
#晚期NSCLC#
54
#联合化疗#
67
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
90