JAMA Network Open:食管癌患者放化疗与胸椎骨折的关系
2020-09-04 liangying MedSci原创
放化疗与食管癌患者的胸椎骨折有关。减少对胸椎的辐射剂量可减少骨折的发生率。
椎体骨折是成人最常见的骨质疏松性骨折。年龄、性别、体重指数、骨质疏松性骨折史、吸烟史、口服糖皮质激素史、饮酒史、父母髋部骨折史、HU值过低被认为是椎体骨折的危险因素。椎体骨折降低了病人的活动能力和生活质量,增加了死亡率。
曾有很多研究报道,恶性肿瘤的放疗与椎体骨折有关。如胰腺癌术前放化疗(CRT)、局部晚期非小细胞肺癌放疗以及脊柱肿瘤的立体定向放射治疗后1 ~ 2年的椎体骨折累积发生率为8% ~ 19%。这些椎体骨折的发生率高于一般骨质疏松性骨折。
然而,在那些证明放疗与椎体骨折相关的报告中普遍存在两个关键缺陷。首先,这些报告是仅基于测量接受放疗的患者的发病率的研究。他们的报告中没有设置对照组,未能削弱混杂因素的影响,如恶性肿瘤(这是脊椎骨折的一个危险因素)。其次,以前的报道没有考虑胸椎骨折的倾向性。胸椎骨折常发生在第7、8、11或12椎体,这些报告没有分析照射野或照射剂量与椎体骨折位置的关系。
基于这些情况,食道鳞状细胞癌被认为适合用于评估放射治疗与胸椎骨折的相关性。第一,与胃食管交界处的腺癌不同,鳞状细胞癌起源于胸段食管。其治疗是多模式的,包括内窥镜治疗、手术和肿瘤同步放化疗(CRT)。这一特征使williamhill asia 能够比较这些接受放射治疗的患者的椎体骨折发生率。第二,食管癌放疗范围广,照射野包括原发肿瘤、转移性纵隔淋巴结及胸段食道,多数胸椎被包括在照射野。这使williamhill asia 能够调查单个椎体的照射剂量与椎体骨折之间是否存在关联。
近日,JAMA Network Open上的一篇研究就探讨了食管癌患者放化疗与胸椎骨折的关系。这项回顾性队列研究纳入了2007年1月1日至2013年12月31日在日本京都大学医院就诊的临床I ~ III期胸段食管癌患者。分析了2018年4月6日至2020年6月4日的数据,研究主要结局是36个月内胸椎骨折的累积发生率。在多变量分析中探讨可能的危险因素,包括CRT,对放射剂量与椎骨骨折的关系也进行了评估。
纳入分析的315例患者中位年龄为65岁(范围32-85岁);56名(17.8%)为女性;男性患者259人(82.2%)。中位观察时间总体为40.4(0.7-124.1)个月,CRT组为40.3(4.0-122.7)个月,非CRT组为40.6(0.7-124.1)个月。
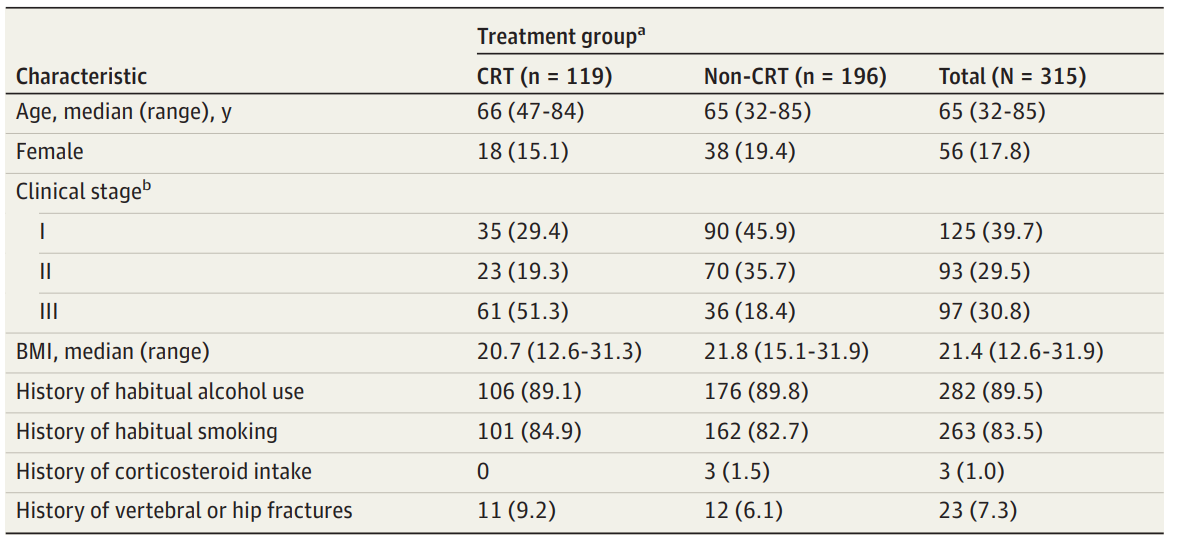
患者基线特征
研究结果显示,放化疗组36个月胸椎骨折累计发生率为12.3% (95% CI: 7.0%-19.1%)。与非CRT组(3.5% [95% CI, 1.3%-7.5%])相比,CRT组胸段椎体骨折的累计发生率更高。
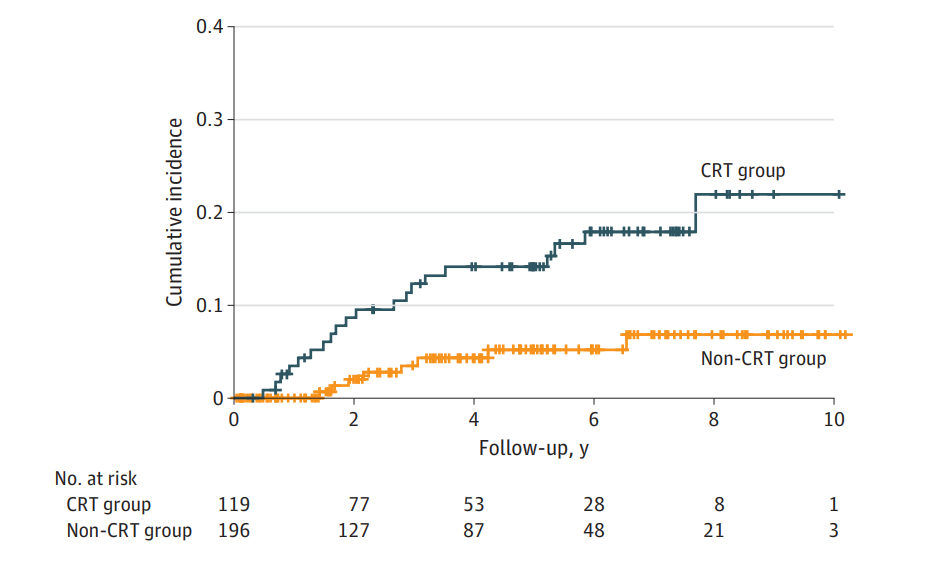
胸段椎体骨折的累积发生率
多变量分析显示,经性别调整后,CRT组与非CRT组胸椎骨折的HR为3.91(95%CI,1.66-9.23;P=0.002),经年龄调整后的HR为3.14(95%CI,1.37-7.19;P=0.007),校正椎体或髋部骨折史的HR为3.10(95%CI,1.33-7.24;P=0.009)。胸椎骨折对单个椎体的平均辐射剂量增加5 gy时的HR为1.19(95%CI,1.04-1.36;P=0.009)。
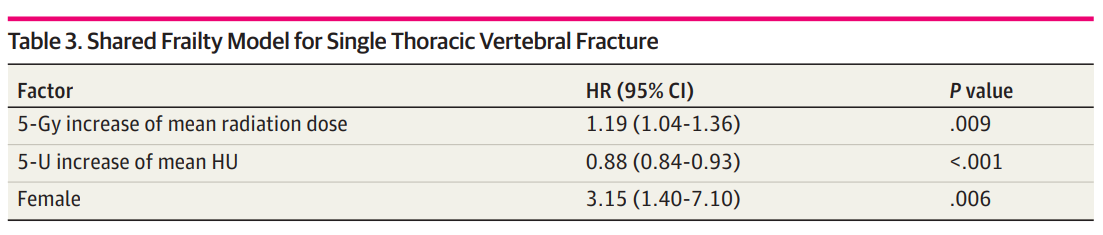
单一胸椎骨折shared frailty模型
本研究是第一个对I ~ III期食管癌患者行内镜、手术或CRT治疗后胸椎骨折发生率进行调查的研究。研究结论显示,与接受内窥镜治疗或手术的患者相比,接受CRT治疗的患者更易发生胸椎骨折。CRT组椎体骨折的累计发生率与既往放疗后椎体骨折的报道一致。目前的分析包括了已知的椎体骨折危险因素,并确定CRT是胸椎骨折的独立危险因素。研究结果中3年累计椎体骨折发生率为12.3%,说明CRT治疗胸段食管癌后椎体骨折并不少见。
放射治疗所致骨折的病理生理机制与老年性骨质疏松的病理生理机制相似。其特征是成骨细胞介导的骨形成减少,骨髓脂肪增多,骨细胞凋亡。这些变化导致骨骼结构的恶化,骨密度的丧失,最终导致椎体骨折。
为了降低椎体骨折的风险,可以对这一人群进行口服维生素D或钙片等治疗。对低HU椎体的自动轮廓识别系统和减少对这些椎体的辐射剂量将是未来放射治疗计划的工作。(CT值是测定人体某一局部组织或器官密度大小的一种计量单位,通常称亨氏单位(hounsfieldunit,HU)空气为-1000,致密骨为1000。)
参考文献:Fujii, K., Sakanaka, K., Uozumi, R., Ishida, Y., Inoo, H., Tsunoda, S., … Mizowaki, T. (2020). Association of Chemoradiotherapy With Thoracic Vertebral Fractures in Patients With Esophageal Cancer. JAMA Network Open, 3(9), e2013952. doi:10.1001/jamanetworkopen.2020.13952
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#食管癌患者#
58
#NET#
45
#PE#
52
#放化疗#
45
#食管#
51
#胸椎#
47
学习了
88
好
105
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
50