Gastroenterology:隐性恶性粘膜下浸润癌高风险因素
2017-06-05 zhangfan MedSci原创
通过对2106名内镜黏膜切除术患者的数据分析确定隐性恶性粘膜下浸润癌高风险因素,该研究助于临床医生根据患者病情特点选择适当的治疗手段
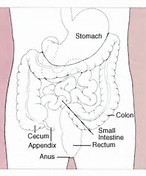
对于结直肠大息肉或侧扩展病变的患者,确定粘膜下浸润癌(SMIC)的风险十分必要。研究认为对于高隐蔽性病变SMIC患者进行内镜下黏膜下剥离术(ESD)比内镜黏膜切除术(EMR)效果更好。近日研究人员通过无明显内镜高危征象病变检查确定隐蔽SMIC相关风险因素。
研究人员分析了2008年至2016年间的进行EMR的大肠无蒂、平坦大肠息肉或侧向扩散病灶患者,收集患者和病变的特点,处置手段和组织学检查结果。
研究共对2106名患者(平均年龄67.7岁,53.2%男性)的2277例组织样本(平均大小36.9mm)进行分析,发现SMIC171例(7.6%),相关风险因素包括工藤腺管开口形态(0–IIc),直肠乙状结肠定位,非颗粒状表面形貌和息肉体积增大。随着SMIC 病变明显,隐蔽SMIC相关因素是直肠乙状结肠定位(OR,1.87;P =0. 01),表面形貌(OR,3.96–22.5)和息肉大小增加(OR 1.16/10 mm; P=0.012)
本研究通过对2106名内镜黏膜切除术患者的数据分析确定隐性恶性粘膜下浸润癌高风险因素,该研究助于临床医生根据患者病情特点选择适当的治疗手段。
原始出处:
DR Nicholas G. Burgess et al. Risk Stratification for Covert Invasive Cancer Among Patients Referred for Colonic Endoscopic Mucosal Resection: A Large Multi-center Cohort. Gastroenterology. June 2 2017.
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#粘膜#
44
#GAS#
41
#AST#
51
#高风险#
51
#Gastroenterol#
0
#Gastroenterology#
37
学习了,谢谢分享
61
研究认为对于高隐蔽性病变SMIC患者进行内镜下黏膜下剥离术(ESD)比内镜黏膜切除术(EMR)效果更好。
70