Br J Cancer:CYP3A7 rs45446698 SNP:绝经前的雌酮和孕酮水平与激素受体阳性乳腺癌患病风险的相关因素
2021-02-02 xiaozeng MedSci原创
流行病学相关研究目前为体内激素在乳腺癌的病因学中的作用提供了有力的证据。
流行病学相关研究目前为体内激素在乳腺癌的病因学中的作用提供了有力的证据。前瞻性研究数据汇总分析显示,在绝经后妇女中,体内循环中的雌二醇或雌酮的倍增与乳腺癌风险增加相关,约升高30-50%左右,而绝经前妇女的患乳腺癌风险增加20-30%。
既往研究显示,绝经前的孕激素水平与患乳腺癌的风险相关。先前的研究已筛选642个相关的SNP,包括涉及类固醇合成或代谢的42个基因,并测试了与绝经前的尿雌酮-3-葡糖苷酸和孕二醇-3-葡糖苷酸的相关性。
雌酮-3-葡糖苷酸和孕二醇-3-葡糖苷酸分别是雌激素和孕激素的尿代谢产物,该研究旨在鉴定与尿液中的性激素水平以及乳腺癌患病风险相关的遗传突变。
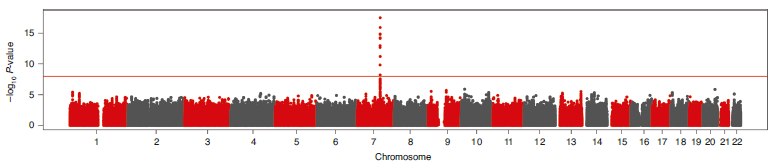
SNP与雌酮-3-葡糖苷酸水平的曼哈顿图
研究人员对560名绝经前妇女的尿雌酮-3-葡糖苷酸和孕二醇-3-葡糖苷酸水平进行了全基因组关联研究,并进一步的分析了298名绝经前妇女的孕酮水平。为了测试与乳腺癌风险的关联性,研究人员对乳腺癌协会的90,916例病例和89,893例对照进行了基因分型分析。以上选取的均为欧洲人样本。
结果显示,对于孕二醇-3-葡糖苷酸,并无全基因组范围内的显著关联性。而对于雌酮-3-葡糖苷酸,研究人员鉴定了一个CYP3A基因座的单峰映射,并注释为rs45446698。
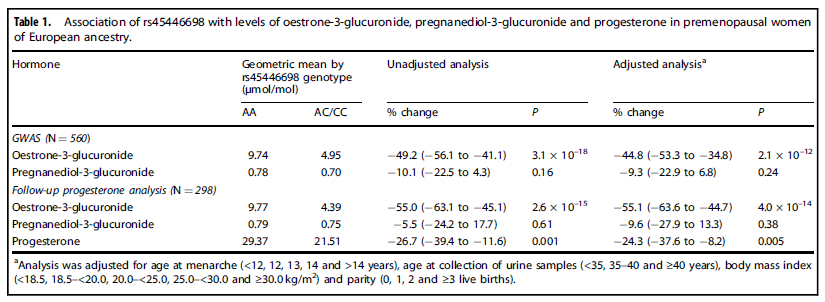
绝经前女性rs45446698与雌酮-3-葡糖苷酸、孕二醇-3-葡糖苷酸以及孕酮水平的关系
研究显示,rs45446698-C等位基因与较低的雌酮-3-葡糖苷酸水平相关;在随访分析中,rs45446698-C等位基因还与较低的孕激素水平、雌激素和孕激素受体阳性乳腺癌低风险相关。
总而言之,CYP3A7基因上的rs45446698 C等位基因与激素受体阳性的乳腺癌患病风险降低相关,该相关性可能是通过影响绝经前女性内源性激素的代谢所引起的。
原始出处:
Johnson, N., Maguire, S., Morra, A. et al. CYP3A7*1C allele: linking premenopausal oestrone and progesterone levels with risk of hormone receptor-positive breast cancers. Br J Cancer (26 January 2021).
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














#激素受体阳性#
112
#绝经前#
72
#绝经#
67
#患病风险#
82
#SNP#
81
#相关因素#
79
#孕酮#
66