JAMA:CRP指导、7天或14天抗生素方案用于治疗革兰氏阴性菌血症
2020-06-03 MedSci原创 MedSci原创
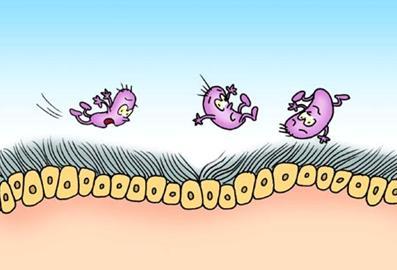
对于革兰氏阴性菌血症的成人患者,CRP指导的抗生素治疗方案、7天治疗方案与14天治疗方案相比,30天临床疗效无显著差异
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言





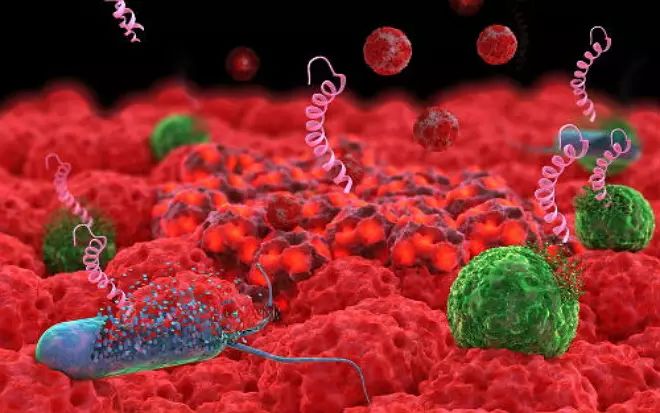




#革兰氏#
68
#CRP#
57
#菌血症#
82
#革兰氏阴性菌#
75
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
87