Cancer Med:研究发现高BMI和既静脉血栓栓塞症史是可切除胃癌患者术前化疗期间发生静脉血栓栓塞症的独立风险因素
2021-07-25 MedSci原创 MedSci原创
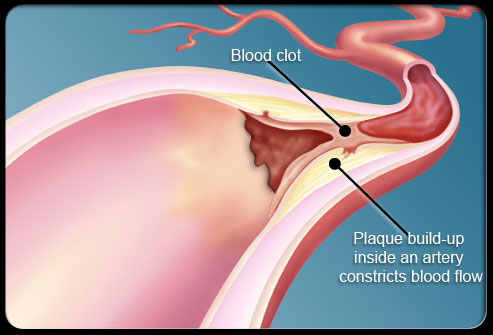
静脉血栓栓塞症(VTE)在癌症患者中很常见,胃癌是VTE的常见危险因素。化疗,尤其是顺铂,与VTE的发生密切有关。在这项研究中,研究人员调查了CRITICS胃癌试验中接受术前化疗的患者进行了VTE发生
静脉血栓栓塞症(VTE)在癌症患者中很常见,胃癌是VTE的常见危险因素。化疗,尤其是顺铂,与VTE的发生密切有关。在这项研究中,研究人员调查了CRITICS胃癌试验中接受术前化疗的患者进行了VTE发生的危险因素及其对后续治疗干预的潜在影响,研究结果已发表Cancer Med。
研究纳入了可切除的胃癌患者,在术前接受三个周期的表柔比星、顺铂或奥沙利铂和卡培他滨(ECC/EOC)治疗。VTE被定义为静脉系统中的血栓,不包括浅表和/或设备相关的VTE。在多变量回归模型中分析了潜在的风险因素,将年龄、性别、身体质量指数(BMI)、肿瘤定位、劳伦分类、化疗类型(ECC/EOC)、(心血管)合并症和以前的VTE作为独立风险因素。研究了VTE对术前化疗完成率、手术切除率、术后并发症和术后治疗开始的影响。
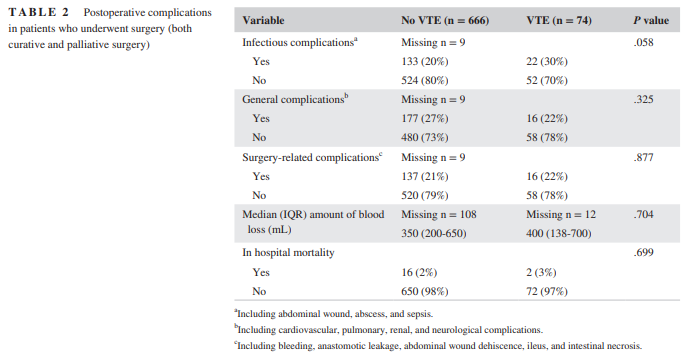
结果显示,781名患者中,有78人(10%)在术前化疗期间发生了VTE。在多变量分析中,BMI≥30 kg/m2和既往VTE史与VTE的发生相关(参考BMI<25 kg/m2;OR 2.190;95% CI 1.152-4.164;P=0.017/既往VTE史;OR 3.617;95% CI 1.201-10.890;P=0.022)。与奥沙利铂相比,顺铂治疗与VTE发生无明显关联(OR 1.535;95% CI 0.761-3.094;P = .231)。VTE的发生并不影响术前化疗的完成,手术切除率,术后并发症,或术后治疗的开始。
综上,该研究结果表明,高BMI和既往VTE史是可切除胃癌患者术前化疗期间发生VTE的独立风险因素。术前发生的VTE并不影响接受进一步治疗。
原始出处:
Astrid E Slagter, et al., Venous thromboembolism during preoperative chemotherapy in the CRITICS gastric cancer trial. Cancer Med. 2020 Sep;9(18):6609-6616. doi: 10.1002/cam4.3118.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#栓塞症#
67
#胃癌患者#
70
#研究发现#
62
#静脉#
58
#静脉血#
65
学习了,谢谢分享
82
#Med#
56