Sci Rep:不同类型胰腺癌细胞中KRAS突变的异质性
2017-08-22 王婳婳 BioArt
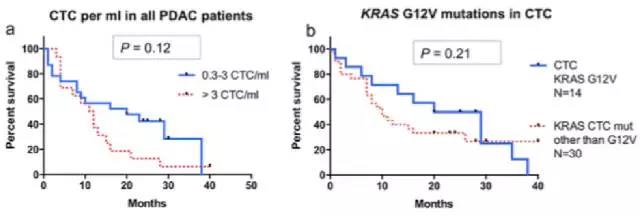
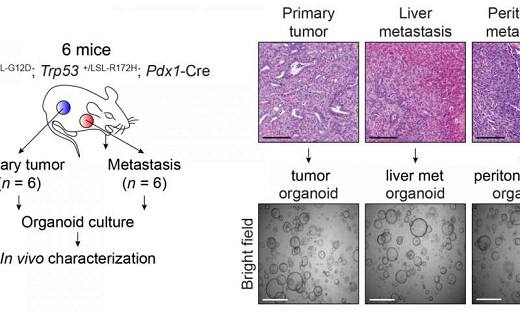
胰腺导管腺癌(PDAC)是一种破坏性疾病,血液中的循环肿瘤细胞(CTC)被认为是全身肿瘤扩散的手段。PDAC是美国和欧洲癌症相关死亡的第四大原因,发生率几乎等于死亡率,5年生存率<6%。这主要是由于其在转移期经常晚期诊断,具侵袭性,并仅对部分已知化学疗法应答。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#不同类型#
46
#癌细胞#
55
#KRAS突变#
59
#KRAS#
46
#RAS突变#
43
非常好的文章.学习了.很受益
77
学习谢谢分享
65
学习了谢谢分享
61
谢谢了.学习
73
学习了
69