Investigative Radiology:使用BOLD成像模型实现心肌组织氧合及微血管血容量的无创测量
2022-09-10 shaosai MedSci原创
血氧水平依赖性信号是由Ogawa等学者首次报道的,已经彻底改变了脑功能成像的流程及格局。
 现阶段,心血管磁共振成像(MRI)已被广泛用于评估心肌的宏观结构和微观结构,许多研究已经证明了绘制心肌参数图的临床价值。另一种评估重要血液动力学变化的方法是使用血氧水平依赖性(BOLD)对比。血氧水平依赖性信号是由Ogawa等学者首次报道的,已经彻底改变了脑功能成像的流程及格局。
现阶段,心血管磁共振成像(MRI)已被广泛用于评估心肌的宏观结构和微观结构,许多研究已经证明了绘制心肌参数图的临床价值。另一种评估重要血液动力学变化的方法是使用血氧水平依赖性(BOLD)对比。血氧水平依赖性信号是由Ogawa等学者首次报道的,已经彻底改变了脑功能成像的流程及格局。
有研究表明,狭窄的冠状动脉远端微血管处于血管扩张的基础状态,并可能在糖尿病、非缺血性扩张型心肌病、冠状动脉狭窄、心脏移植排斥和淀粉样变等疾病状态下受到影响。研究表明,微血管血容量(MBVs)的测量是一项重要的组织特征。
最早的心肌BOLD研究是在动物呼吸和孤立的灌注心脏模型中进行的。在一份评估心肌BOLD信号生理基础的早期手稿中,Atalay证明了在孤立的灌注兔心脏恒定血流条件下,T2和血液中血红蛋白氧饱和度之间的强烈相关性。在后来的研究中,人类志愿者的心肌BOLD信号在基线和由多巴胺或双嘧达莫诱导的心肌应激过程中被显示出来。
近日,发表在Investigative Radiology杂志的一项研究提出了一个可以定量测量药物诱导的微血管容积变化的BOLD MRI模型,并使用BOLD MRI测量了药物诱导的组织氧合变化,为早期识别心肌的微观病理变化、实现早期干预及治疗提供了技术支持。
本研究使用了12只健康大鼠进行研究。在输注增加微血管血流的腺苷或增加心肌耗氧量的多巴胺的情况下获取R2*maps。此外,在静脉注射单晶氧化铁纳米粒子后,在注射及不注射腺苷或多巴胺的情况下获取R2*maps。
结果显示,使用腺苷时,微血管总体积增加了10.8%,使用多巴胺时增加了25.6%(P<0.05)。当比较心内膜与心外膜时,腺苷和多巴胺都显示心内膜和心外膜的MBV变化有明显差异(P < 0.05)。腺苷的心肌总氧饱和度增加了6.59%,多巴胺增加了1.64%(P = 0.27)。每种药物的心外膜和心内膜氧饱和度变化的差异都很明显(腺苷P < 0.05,多巴胺P < 0.05)。

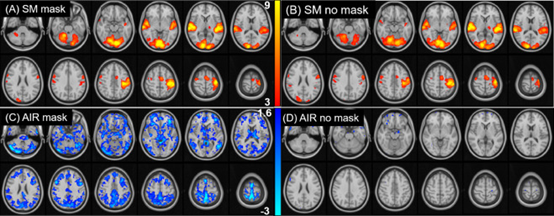
图 大鼠心肌的R2*maps。A,静息状态。B,腺苷输注期间。C,单晶铁氧化颗粒(MION)给药后,未注射腺苷。D,使用MION后,并注射腺苷
本研究结果证明了使用校准的血氧水平依赖性MRI来量化微血管容积和氧合变化的能力,并证明了腺苷和多巴胺使用下的不同反应。本研究提出的方法在检查各种疾病状态下的微血管疾病方面具有较大的临床潜力,且无需使用任何放射性药物或钆基造影剂,安全性及实用性进一步得到提升。
原文出处:
Jeffrey M Dendy,Sean G Hughes,Jonathan H Soslow,et al.Myocardial Tissue Oxygenation and Microvascular Blood Volume Measurement Using a Contrast Blood Oxygenation Level-Dependent Imaging Model.DOI:10.1097/RLI.0000000000000871
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#EST#
74
#血容量#
83
#微血管#
115
#IgA#
108