Nutrients:在慢性他汀类药物治疗患者中,补充二十八烷醇会影响PCSK9水平并恢复其与 LDL-C的生理关系
2021-10-18 “心关注”公众号 “心关注”公众号
关于多廿烷醇(单独或与他汀类药物联合使用)的降脂作用数据存在矛盾,在一些高质量研究中,其是否对血清低密度脂蛋白胆固醇(LDL-C)水平具有任何有利影响尚存疑虑。目前还不清楚是否因为基因差异导致了这种结
关于多廿烷醇(单独或与他汀类药物联合使用)的降脂作用数据存在矛盾,在一些高质量研究中,其是否对血清低密度脂蛋白胆固醇(LDL-C)水平具有任何有利影响尚存疑虑。目前还不清楚是否因为基因差异导致了这种结果的多样性,但在当前的欧洲血脂异常管理威廉亚洲博彩公司 中,对多廿烷醇的使用一直处于不鼓励态度。尽管如此,作为一种膳食补充剂它在世界各地仍被普遍使用(单独使用或与不同的营养药物结合使用)。
PCSK9抑制剂在过去十多年中受到了广泛关注。PCSK9是一种蛋白酶,可促进LDL受体(LDLr)的溶酶体降解,从而调节循环中LDL-C的数量。该作用机制启发了新一代药物(PCSK9抑制剂)的研发,该药物可有效阻断PCSK9- LDLr的相互作用,并将降低高达70%的LDL-C水平。此外,他汀类药物与PCSK9相互作用的研究显示,他汀类药物治疗导致血清PCSK9水平升高,这解释了他汀类药物全面降脂作用的降低。有趣的是,已有研究表明,在开始接受他汀类药物治疗的患者中,二十八烷醇可能阻止PCSK9水平的上升,并降低其在健康人群中的水平。此外,一些保健品可能会降低动物和人类的PCSK9水平。营养药物,如小檗碱和姜黄素,可能通过SREBP(固醇调节元件结合蛋白)非依赖性途径抑制PCSK9的表达。相反,他汀类药物通过激活SREBP-2增加PCSK9的表达,这可能会减弱其有益作用。然而,目前尚不清楚PCSK9水平升高(与LDL-C值无关)是否为发生心血管事件的独立危险因素。即使是最近批准的抑制PCSK9合成的新药物Inclisiran(慢干扰RNA, siRNA)也存在这个问题,因为它是在他汀类药物的基础上使用的。
因此,研究人员进行了一项前瞻性、单中心、随机、双盲、安慰剂对照试验,研究了膳食补充剂(含有二十八烷醇[20 mg]和维生素K2-MK7[45 μg])是否可能影响慢性他汀类药物治疗患者中PCSK9的水平及其与LDL-C的关系。
方法
2015年11月至2016年6月,在一项随机、双盲、安慰剂对照试验中,受试者被分配每天服用一粒膳食补充剂或安慰剂。膳食补充剂和安慰剂由AbelaPharm(贝尔格莱德,塞尔维亚)生产和提供。膳食补充剂含有二十八烷醇(20 mg)和维生素K2-MK7(45μg)。安慰剂胶囊在外观(颜色、形状、质地)和味道上与补充剂相同,但其是由硬脂酸镁、微晶纤维素和胶体二氧化硅组成。应用剂量为20 mg的二十八烷醇相当于约30 mg的多廿烷醇。
受试者被要求避免使用维生素K和对LDL-C及甘油三酯水平产生干扰的膳食补充剂。建议的低脂饮食和其他药物治疗通过在基线和研究结束时的3天食物/药物记录进行监测。在基线、8周和13周后对患者进行检查和血液分析。在第5周和第10周,对患者进行关于不良反应的调查。患者依从性定义为摄入至少85%的预定胶囊,这将在第8周和第13周结束时由返回的胶囊数量验证。
结果
根据纳入/排除标准,共筛选出177例患者,最终纳入87例患者。在87例患者中,45例(51.7%)和42例(48.3%)被随机分配,分别接受为期13周的安慰剂或膳食补充剂。6例患者在研究终点前退出,5例来自膳食补充剂组,1例来自安慰剂组,原因是与研究无关的个人原因和胃痛。(图1)
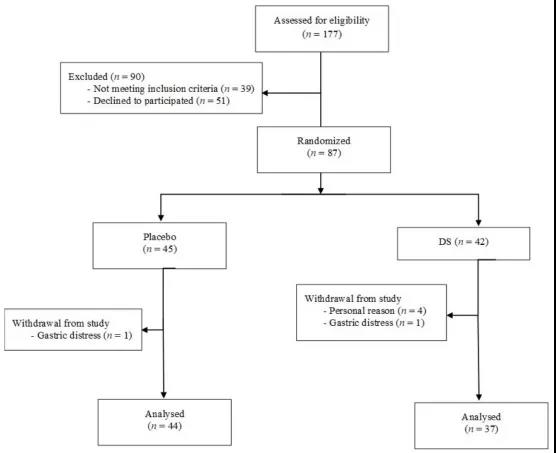
图1.研究流程图
患者平均年龄为62.6±0.8岁,男性占63.2%。平均BMI为27.6±0.4。超过半数(52.9%)患者有冠心病家族史,所有患者均有血脂异常史。总体而言,高血压、糖尿病和当前吸烟者分别占研究人群的96.6%、26.4%和24.1%。分别有60%和62%的患者存在心肌梗死和心肌血运重建术(主要通过支架)。两组之间在人口统计学、体脂参数、吸烟状况或任何临床变量方面均无显着差异。除TG水平(安慰剂组较高,P <0.05)外,两组大部分生化指标均无显着差异。患者依从性为97%。(表1)
表1.基线特征
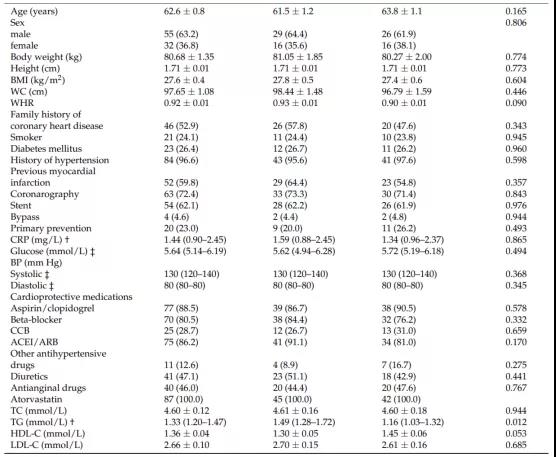
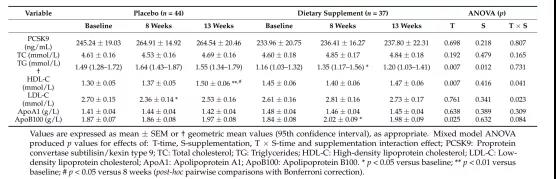
表2显示了基线时、第8周和13周后的血清PSCK9水平和血脂参数。两组PCSK9水平在研究期间保持不变。两组患者的甘油三酯和载脂蛋白A1水平在研究期间均无显着变化。与基线相比,安慰剂组8周后的LDL-C水平出现统计学意义下降(补充和时间的交互作用,P =0.023),但在13周后这种作用消失。安慰剂组的基线血清甘油三酯水平显着高于膳食补充剂组(P =0.012)。补充膳食剂组在8周后血清甘油三酯水平较基线显着升高(主要影响因素为时间,P =0.007),但在13周后影响消失。在接受膳食补充剂治疗的13周期间,未观察到HDL-C值与基线值相比变化,而安慰剂组HDL-C值有所增加(P <0.001,Bonferroni后续检验)。与基线相比,膳食补充剂组8周后血清载脂蛋白B100水平显着升高(但临床无相关性),但在13周后影响消失(主要影响因素为时间,P =0.025)。
表2. 基线、8周和13周后的血清PSCK9和血脂参数
在膳食补充剂组中,8周后即刻观察到PCSK9水平的百分比变化与LDL-C水平的百分比变化之间存在显着正相关(R=0.383,P =0.019),且该变化持续至第13周,即从基线到终点(R=0.409, P =0.012)。(图 2A、C)
在安慰剂组中未观察到这种相关性(第 8 周R=0.078,P =0.615;第 13 周R= -0.103,P =0.508)。(图 2B、D)。
因此,在膳食补充剂组,PCSK9 水平下降幅度最大往往血清 LDL-C 水平下降幅度也最大。
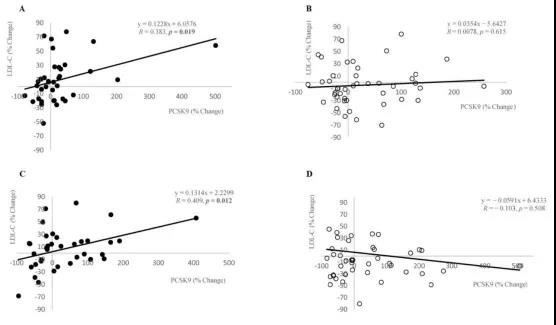
图2. 比较8周和13周时阿托伐他汀诱导的血清PCSK9与LDL-C水平百分比变化
图3A显示了这些参与者从基线到终点的血清PCSK9水平变化。到治疗期结束时,两组患者的PCSK9水平未见明显改变。然而,这两种治疗方法的效果是不同的。在这两个亚组中,PCSK9基线水平具有可对比性:膳食补充剂组为236.26±31.48 ng/mL,安慰剂组为241.11±25.34 ng/mL(P >0.05)。然而,在第13周结束时,膳食补充剂组的PCSK9水平显着降低(安慰剂组为280.33±33.96,补充剂组为191.47±25.85;P =0.077)。
图3B显示了在研究期间发生不利脂质变化的受试者的PCSK9水平。在膳食补充剂组和安慰剂组中均未观察到 PCSK9 水平的显着变化。

图3. LDL-C和HDL-C发生有利变化,LDL-C和HDL-C发生不利变化的患者基线和补充13周后的血清PCSK9水平
结论
该研究表明,膳食补充剂可以恢复被他汀类药物治疗中断的PCSK9和LDL-C水平之间的生理正相关关系。使用他汀类药物治疗可能导致PCSK9升高,PCSK9与LDL-C水平呈负相关。考虑到自发和/或药物诱导的PCSK9水平升高可能是一个独立的健康危险因素,该研究的发现可能具有临床相关性。
原始出处:
Ciric Milica Zrnic et al. Supplementation with Octacosanol Affects the Level of PCSK9 and Restore Its Physiologic Relation with LDL-C in Patients on Chronic Statin Therapy.[J]. Nutrients,2021,13(3).
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#Csk#
65
#PCS#
75
#他汀类药#
52
#LDL#
58
文章内容与生活息息相关,值得阅读
85