真实世界研究表明:通络药物治疗心血管病现曙光
2018-03-17 佚名 医学界心血管频道
“3月17日,第十四届国际络病学大会在济南召开。上海长征医院吴宗贵教授、海军军医大学附属长征医院的梁春教授、中国医科大学附属第一医院曾定尹教授介绍了通络药物在真实世界中研究成果。
“3月17日,第十四届国际络病学大会在济南召开。上海长征医院吴宗贵教授、海军军医大学附属长征医院的梁春教授、中国医科大学附属第一医院曾定尹教授介绍了通络药物在真实世界中研究成果。
来自上海长征医院的吴宗贵教授在“冠心病与动脉粥样硬化”分论坛上介绍了中药通心络胶囊治疗心绞痛真实世界研究概况。
吴宗贵教授在会议现场,真实世界研究的大数据
吴教授指出,这项研究在全国28个地区的1000余家医院中开展,收集了23340例心绞痛患者,涵盖了劳累性心绞痛、自发性心绞痛、混合性心绞痛等多种临床常见的发病类型,许多患者伴有糖尿病、高血压、血脂异常、脑卒中等重大疾病,与现实生活中心脑血管病患者多为“三高”的情况一致。
患者在接受抗凝、降脂、扩冠等基础治疗上加服通心络胶囊,结果发现服用通心络胶囊后患者缓解心绞痛的疗效提高了25.3%,缓解胸闷的疗效提高了28.3%,心电图ST段下斜性下移幅度明显改善;患者的肢体活动、心绞痛稳定状态、心绞痛发作情况、治疗满意度均得到不同水平的改善。
一个中药开展范围如此之广、涉及医院之多、研究项目之丰富的真实世界研究,在我国实属罕见。
通络药物对心血管病的真实作用
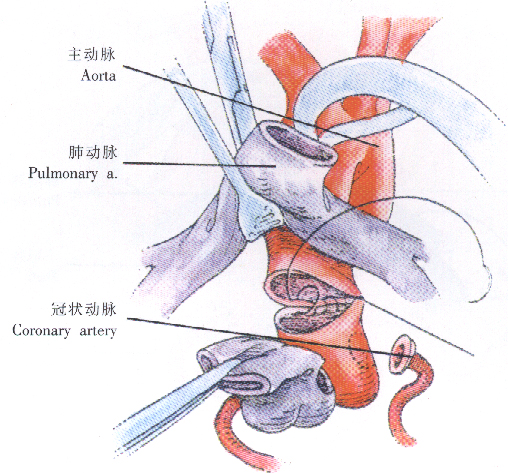
冠状动脉粥样硬化斑块是冠心病发生的主因。斑块形成会使血管腔变窄,使血液流动的阻力变大,血流速度变缓,心脏血液供给不足。斑块破裂还会形成血栓,完全堵塞血管,切断器官组织的血液供应,致使突发心梗等急性心血管事件。海军军医大学附属长征医院的梁春教授在络病学大会上报告了最新研究成果,通心络能够降低斑块内脂质的质量,从而起到稳定和逆转斑块的作用。
血管痉挛是血管壁剧烈收缩,引起血管腔变窄,甚至完全闭合,引发心绞痛,有时还会导致血管壁上的斑块破损、脱落,形成的血栓堵塞血管,引发心梗。中国医科大学附属第一医院曾定尹教授在会议报告中指出,通心络可通过干预血管内、外膜的两种机制防治冠状动脉痉挛,进而治疗心绞痛,内膜参与机制是调节一氧化氮/内皮素(ET)-1平衡,外膜参与机制是抑制Rho激酶活性。多途径、多靶点缓解冠状动脉痉挛改善变异型心绞痛的特点,使通心络成为中华医学会心血管病分会《冠状动脉痉挛性疾病的诊断与治疗中国专家共识》推荐的中成药。
微血管损伤在心血管病发病过程中扮演重要角色。心梗后心肌微血管多会受损,即使支架术后大血管再通,也常常引起再灌注后心肌无复流,这是医学界的难题。以通心络胶囊为主要药物的“新三联”治疗方案,即通心络+负荷他汀+尼可地尔,可以保护梗死心肌,减少微血管的无复流,对降低心梗患者的再住院率和死亡率具有重大意义,因此,通心络也是《冠脉微血管疾病诊断和治疗的中国专家共识》的推荐中成药。
真实世界研究是什么?
真实世界研究是国际医学界最新推出的药物疗效研究方法,其特点是客观、科学、真实,能最大限度还原药物临床应用中的真实疗效。一方面,真实世界研究不限制入组患者的年龄、性别、病情,这就确保了研究对象和现实中的患者具有高度的一致性。另一方面,真实世界研究的数据来源非常广泛,除了收集传统临床研究重视的医院门诊、住院病历记录的症状、化验指标外,还会收集医保部门、民政部门、公共卫生部门日常监测、记录、储存的各类与健康相关的数据。
随着科技的发展,患者通过可穿戴智能设备监测的心率、血压、心电图等健康记录也被真实世界研究收集,通过海量的数据,分析评价药物在各种现实生活环境影响下表现出来的安全性和有效性。真实世界研究因而被称为药物的“终极大考”。
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#血管病#
47
#曙光#
44
学习了.谢谢作者分享!
107
#真实世界#
47