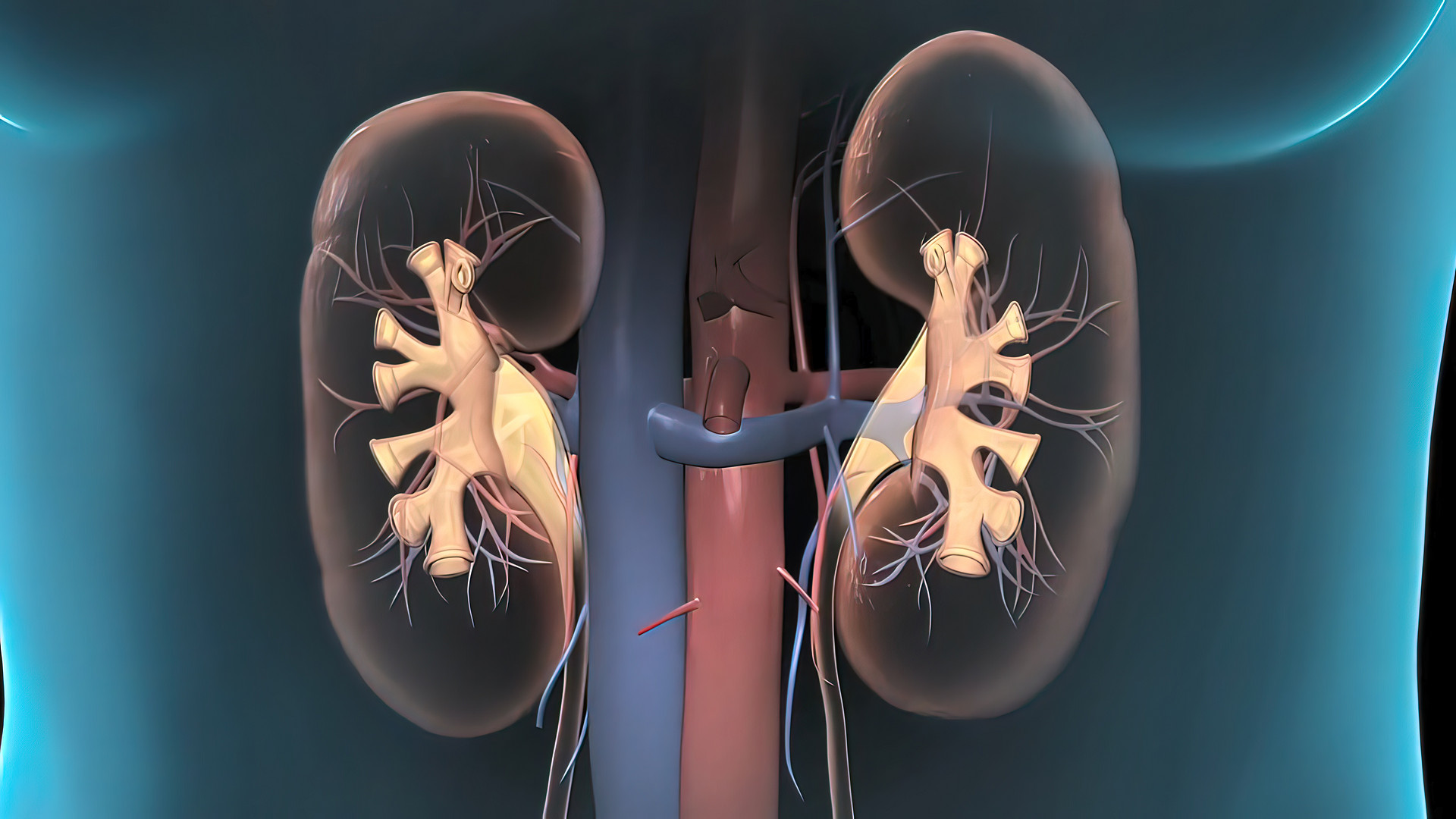
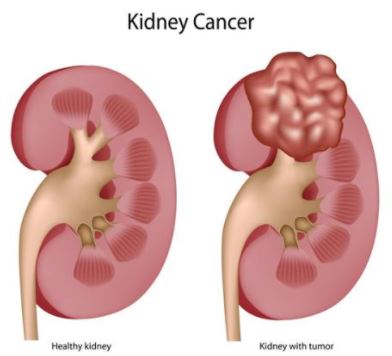
Opdivo(nivolumab)联合Cabometyx(cabozantinib)一线治疗晚期肾细胞癌,CHMP持积极意见
2021-02-27 Allan MedSci原创
Opdivo(nivolumab)联合Cabometyx(cabozantinib)组患者的无进展生存期(PFS)、总生存期(OS)和客观缓解率(ORR)均得到了显著改善。
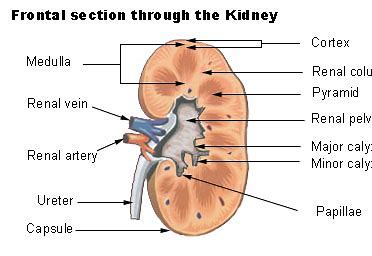
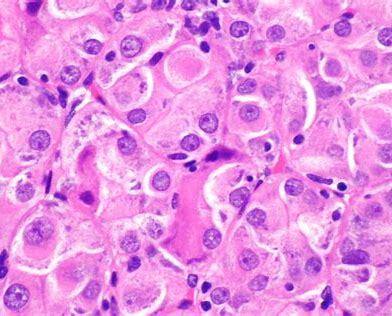
Bristol Myers Squibb今天宣布,欧洲药品管理局(EMA)人用药品委员会(CHMP)已建议批准将Opdivo®(nivolumab)与Cabometyx®(cabozantinib)结合使用一线治疗晚期肾细胞癌(RCC)。
Bristol Myers Squibb泌尿生殖系统癌症发展计划负责人Dana Walker表示:“近年来,肾细胞癌治疗领域发生了转变,许多进步帮助改善了患者预后”。
CHMP的积极意见来自于CheckMate-9ER III期试验的积极结果。结果显示,与舒尼替尼相比,Opdivo(nivolumab)联合Cabometyx(cabozantinib)组患者的无进展生存期(PFS)、总生存期(OS)和客观缓解率(ORR)均得到了显著改善。Opdivo联合Cabometyx的耐受性良好。
CheckMate-9ER是一项开放标签、随机、多中心III期临床试验,旨在评估Opdivo联合Cabometyx在初治晚期或转移性肾细胞癌(RCC)患者中的有效性和安全性。共计招募了651例患者,其中323例患者被随机分配至Opdivo/Cabometyx联合治疗组,328被随机分配至舒尼替尼组。主要终点是无进展生存期(PFS);次要终点包括总生存期(OS)和客观反应率(ORR)。
原始出处:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#细胞癌#
62
#mAb#
56
#NIV#
57
#MET#
60
#CHMP#
83
#Opdivo#
74
#晚期肾细胞癌#
59
#cabozantinib#
67
#ABO#
48