Blood:自体移植 or 异体移植,外周T-NHL患者到底该选谁?
2021-01-05 Nebula MedSci原创
外周T细胞淋巴瘤年轻患者的标准一线疗法包括六个疗程的CHOP或CHOEP后,再用高剂量疗法和自体干细胞移植(AutoSCT)巩固
外周T细胞淋巴瘤年轻患者的标准一线疗法包括六个疗程的CHOP或CHOEP后,再用高剂量疗法和自体干细胞移植(AutoSCT)巩固。Schmitz等推测巩固性异基因造血干细胞移植(AlloSCT)也可改善这类患者的预后,于是开展了本项III期随机试验以进行验证。
本研究招募了104位18-60岁的除了ALK+ALCL之外的淋巴结外周T细胞淋巴瘤患者,涵盖除了1期和aaIPI0分以外的所有分期和所有IPI评分患者。受试患者被随机分组,接受4 x CHOEP和1 x DHAP后继以高剂量疗法和AutoSCT或清髓性预处理和AlloSCT。主要终点是3年无事件存活率(EFS)。
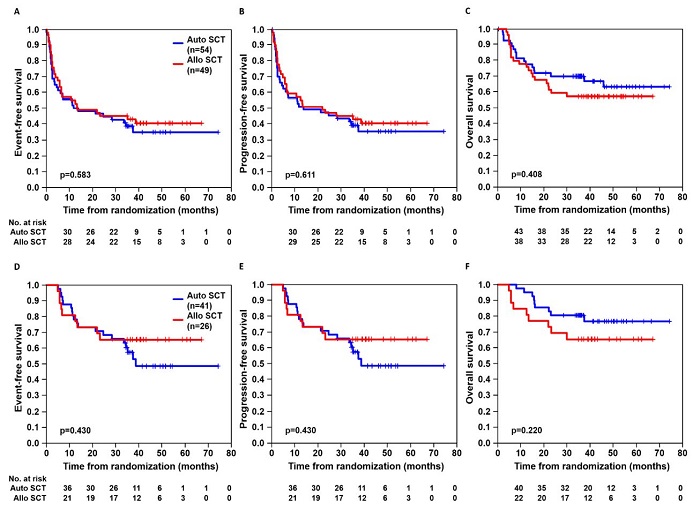
不同治疗组患者的存活预后
中位随访42个月后,接受AlloSCT治疗的患者的3年EFS是43%(95% CI 29%-57%),而接受AutoSCT治疗的患者的是38%(25%-52%);两组的3年总体存活率分别为57% vs 70%,治疗臂间无显著差异。进行AlloSCT的21位患者中没有一人复发,而进行AutoSCT的36位患者中有13人(36%)复发。另外,进行AlloSCT的26位患者中有8位(31%)、进行AutoSCT的41位患者中无一人死于移植相关毒性。
累积(非)复发死亡率
总之,T细胞淋巴瘤年轻患者标准化疗后采用自体干细胞移植或异体干细胞移植进行巩固治疗后的存活预后相对。同种异体移植后移植物抗淋巴瘤的作用被移植相关死亡率所抵消。CHO(E)P继以AutoSCT仍是可移植患者的优先治疗选择。AlloSCT可作为经AutoSCT治疗后复发患者的新选择。
原始出处:
Norbert Schmitz, et al. A randomized phase 3 trial of auto vs. allo transplantation as part of first-line therapy in poor-risk peripheral T-NHL. Blood. December 17, 2020.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














#自体移植#
65
#NHL#
96
#异体移植#
68
GVHD还是一个难题
203
学习了,受益匪浅
192