AR-301治疗COVID-19继发性细菌感染:III期临床试验已开始
2020-05-04 Allan MedSci原创
Aridis Pharmaceuticals是一家专注于开发新型抗感染疗法的生物制药公司,Aridis今日宣布,其AR-301治疗COVID-19继发性细菌感染的III期临床试验的首例患者已经入组。
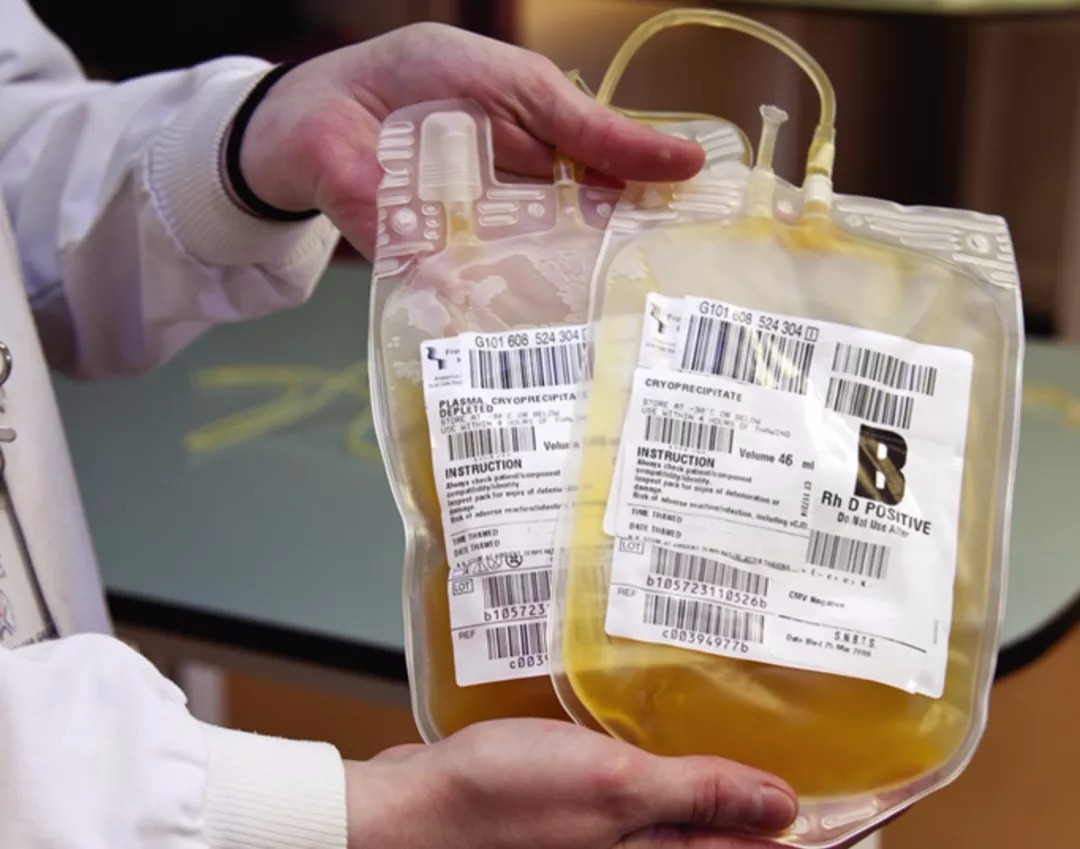
Aridis Pharmaceuticals是一家专注于开发新型抗感染疗法的生物制药公司,Aridis今日宣布,其AR-301治疗COVID-19继发性细菌感染的III期临床试验的首例患者已经入组。AR-301是一种抗金黄色葡萄球菌引起的肺炎的全人源单克隆抗体。
在重症监护病房(ICU)中长时间使用机械通气的COVID-19患者容易受到机会性病原体的继发感染(也称为“超级感染”)。据报道,在COVID-19患者中,超级感染是一种并发症,加剧了COVID-19患者患者的死亡率。Aridis首席执行官Vu Truong表示:“虽然AR-301不能杀灭引起COVID-19的病毒,但它可以缓解继发性金黄色葡萄球菌细菌性肺炎,而继发性细菌感染是COVID-19患者死亡的重要原因”。
这项III期临床研究于2019年第一季度启动,预计将在22个国家的约160个临床中心招募240名患者。
原始出处:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
















#I期临床#
0
#继发#
65
#II期临床试验#
55
#继发性#
57
#III#
56
#I期临床试验#
47
#继发性细菌感染#
42
#细菌感染#
77
#II期临床#
48
#III期临床试验#
51