Clin Cancer Res:突变型IDH1/2双重抑制剂Vorasidenib治疗复发/进展胶质瘤的效果
2021-12-16 MedSci原创 MedSci原创
胶质瘤是最常见的恶性原发性脑肿瘤,其特征是恶性细胞弥漫性浸润大脑,可分为低级别胶质瘤(LGG)和高级别胶质瘤。目前的治疗方案的短期和长期毒性较为显著。但 LGG 进展到更高级别的胶质瘤时,MRI 检查
胶质瘤是最常见的恶性原发性脑肿瘤,其特征是恶性细胞弥漫性浸润大脑,可分为低级别胶质瘤(LGG)和高级别胶质瘤。目前的治疗方案的短期和长期毒性较为显著。但 LGG 进展到更高级别的胶质瘤时,MRI 检查的对比度会增强。
大部分 LGG 患者(约80%)携带异柠檬酸脱氢酶 1 或 2 (IDH1/IDH2) 基因突变。Vorasidenib (AG-881) 是突变型 IDH1/IDH2 酶的一种双重抑制剂,专为改善血脑屏障的渗透而开发,并在 IDH 突变的胶质瘤原位模型中表现出减少肿瘤生长的作用。

Mellinghoff 等研究人员开展了一项多中心、开放标签的、I期剂量递增性试验,探究了 Vorasidenib 在93位携带突变型 IDH1/2(mIDH1/2)的实体肿瘤患者中的剂量和疗效,其中52位是胶质瘤患者,经标准治疗后复发或进展。予以受试患者 Vorasidenib 口服,1/日,28天为一疗程,直到病情进展或出现不可耐受的毒性。
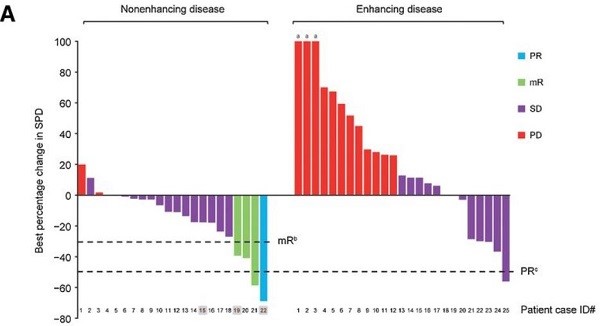
受试患者的缓解情况
研究结果显示,Vorasidenib 在胶质瘤患者队列中的安全性良好。Vorasidenib 剂量≥100 mg 时可见剂量限制性毒性(转氨酶升高),但都是可逆的。根据 LGG 神经肿瘤学反应评估标准,协议定义的非 MRI 增强的LGG患者的客观缓解率为 18%(1例部分缓解,3例小缓解)。
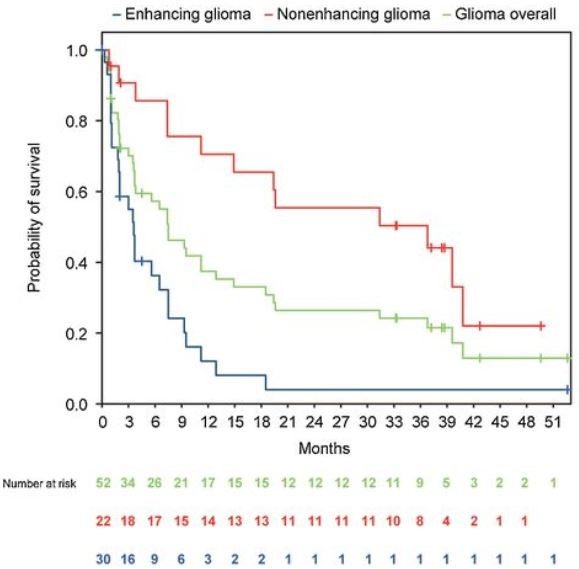
不同亚组患者的存活率
非 MRI 增强的胶质瘤患者的中位无进展生存期为36.8个月,而 MRI 增强的胶质瘤患者的 PFS 为3.6个月。对非 MRI 增强的神经胶质瘤患者的肿瘤体积进行的探索性评估显示,多位患者的肿瘤持续缩小。

患者的肿瘤持续缩小
总而言之,该研究结果显示,Vorasidenib 具有良好的耐受性,并在复发性或进展性非 MRI 增强的 mIDH LGG 患者中显示出初步的抗肿瘤活性。
原始出处:
Ingo K. Mellinghoff, et al. Vorasidenib, a Dual Inhibitor of Mutant IDH1/2, in Recurrent or Progressive Glioma; Results of a First-in-Human Phase I Trial. Clin Cancer Res August 15 2021 27 (16) 4491-4499; DOI:10.1158/1078-0432.CCR-21-0611
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#IDH1#
74
#抑制剂#
35
#突变型#
56
#RASI#
60