HUMAN BRAIN MAPPING:一种探索重度抑郁症患者的脑连接变化的新方法
2021-07-25 MedSci原创 MedSci原创
通过结合结构和功能数据,awFC可以提高或降低区分MDD和HC的不同区域的连通性差异。这种方法可以帮助williamhill asia 更全面地了解结构和功能连接的相互联系的本质,以及其与抑郁症的关系。
对疾病和健康大脑连接模式的日益增长的兴趣导致了多模态成像分析方法的发展,该方法用于将功能磁共振成像(fMRI)数据与扩散张量成像(DTI)数据相结合。多模态成像分析方法旨在捕捉脑网络结构和功能连接之间的复杂相互作用,为脑网络连接提供新的见解。多模态成像分析可以更好地理解人脑连接模式中的关节结构和功能变化。这些方法在识别重度抑郁症(MDD)的大脑网络中断方面可能有临床实用价值。
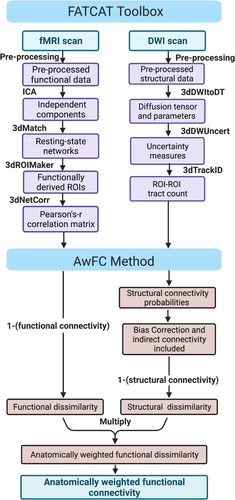
Geoffrey B. Hall将现有的软件工具箱与数学上密集的统计方法相结合,产生了一种新的处理方式,用于快速简便地实现数据融合分析(FATCAT-awFC)。然后利用新的FATCAT-awFC方法识别MDD患者与健康对照参与者(HC)之间的连接(常规功能、常规结构和解剖加权功能连接)变化。
数据来自加拿大抑郁症生物标志物整合网络(CAN-BIND-1)研究。评估了大规模静息态网络。
两组的默认网络和腹侧注意网络的解剖加权功能连接(awFC)的差异具有统计学意义,且影响大小适中(d<0.4)。在默认网络中,一个区域对之间的功能和结构连接似乎在意义上重叠。
FATCAT-awFC保留了结构和功能连接之间关系的复杂性,并提供了最大的信息,同时允许简单的实现。该研究利用FATCAT-awFC方法,期望在常见的RSN中发现MDD患者和HC之间的差异,包括DMN、FPN、DAN、VAN和LIM。假设使用FATCAT-awFC方法进行联合功能结构连接分析,与使用单一模态分析这些变化相比,可以更好地区分MDD组和HC组之间的连接性变化。
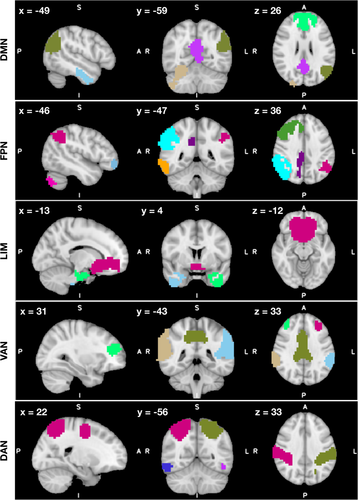
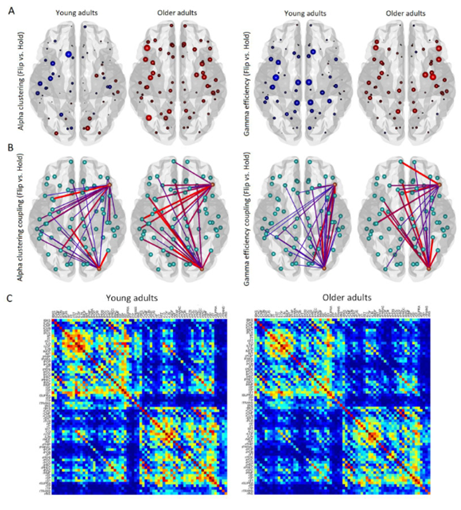
通过对RS fMRI数据的组独立分量分析,得到了静息态网络和相应的感兴趣区域。采用CANBIND-1静息态fMRI数据提取ROIs。从各分量中识别并提取了5个静息态网络(DMN, DAN;FPN;边缘网络;VAN)。所描绘的彩色区域表示每个网络内的不同ROI。
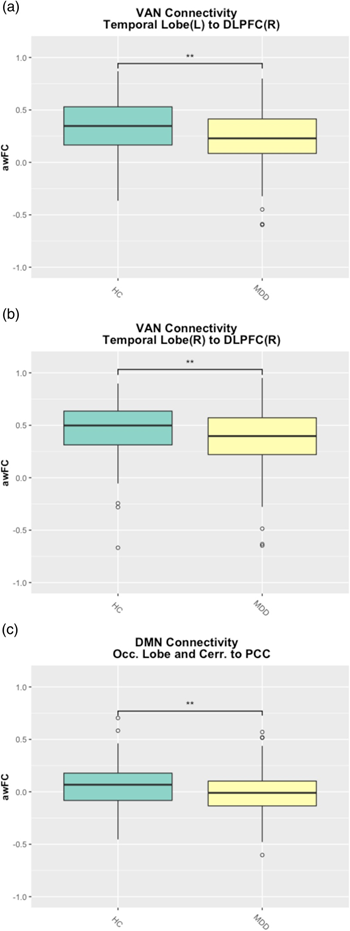
箱图显示重度抑郁症(MDD)ROI对之间的解剖加权功能连接低于健康对照组(HC)受试者。箱线图还量化了MDD和HC组的连接强度(a)VAN内左颞叶和右DLPFC之间的AwFC(b)VAN内右颞叶和右DLPFC之间的AwFC(c)DMN内枕叶/小脑和PCC之间的AwFC。
该研究团队开发了一个结合功能连接(来自fMRI)和结构连接(来自DTI)的新方法,并用它来研究MDD患者awFC连接性的变化。分析了24个ROI(来自5个静息态功能网络),其中3个用FATCAT-awFC方法显示MDD和HC组之间awFC有统计学差异。对于每个区域对,还进行了标准的功能和结构连接分析,以与新的功能-结构组合分析方法(FATCAT-awFC)进行比较。
通过结合结构和功能数据,awFC可以提高或降低区分MDD和HC的不同区域的连通性差异。这种方法可以帮助williamhill asia 更全面地了解结构和功能连接的相互联系的本质,以及其与抑郁症的关系。
原文出处
Exploring brain connectivity changes in major depressive disorder using functional-structural data fusion: A CAN-BIND-1 study. https://doi.org/10.1002/hbm.25590
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#human#
55
#mapping#
50
#新方法#
56
#抑郁症患者#
60