一线治疗晚期肝癌哪家强?《柳叶刀肿瘤学》发布卡博替尼+阿替利珠单抗 vs 索拉非尼III期临床结果
2022-07-06 MedSci原创 MedSci原创
Lancet Oncol :卡博替尼 + 阿替利珠单抗与索拉非尼治疗晚期肝癌(COSMIC-312):一项多中心、开放标签、随机化、3期临床试验
肝细胞癌约占全球肝癌病例的90%。由于肝细胞癌是一种血管生成性肿瘤,因此血管内皮生长因子受体(VEGFR)靶向酪氨酸激酶抑制剂(TKI),改善了各种研究中的生存结局。基于3期SHARP试验,索拉非尼是第一个被批准作为一线治疗的TKI。
随后,免疫检查点抑制剂在肝细胞癌患者中显示出临床益处。在一线治疗中,免疫检查点抑制剂单药治疗可引起一部分晚期肝细胞癌患者的持久肿瘤反应,但在全球随机试验中,总生存期(OS)没有改善。目前已经研究了几种免疫检查点抑制剂组合策略,具有增强抗肿瘤免疫反应的潜力。
将免疫检查点抑制剂与VEGF途径抑制剂和其他免疫调节途径相结合,可以促进免疫许可环境并增强免疫检查点抑制剂的反应。在 3 期 IMbrave150 研究中,与索拉非尼相比,阿替利珠单抗(抗 PD-L1 抗体)加贝伐单抗(抗 VEGFA 抗体)联合使用可改善无进展生存期和总生存期。TKI 和免疫检查点抑制剂组合在几种实体瘤类型中显示出疗效。然而,这种治疗策略尚未在肝细胞癌患者的3期试验中得到评估。因此,COSMIC-312是第一个在这种情况下评估TKI和免疫检查点抑制剂组合的3期试验。
COSMIC-312是一项开放标签、随机、3期临床试验,评估卡博替尼加阿替利珠单抗与索拉非尼一线治疗晚期肝细胞癌患者的疗效和安全性。试验在32个国家的178个中心招募了年龄在18岁及以上的晚期肝癌患者,这些患者不能接受治疗或局部治疗,之前未接受过全身抗癌治疗。允许肿瘤累及包括门静脉在内的主要血管。根据实体肿瘤1.1版(RECIST 1.1)的缓解评估标准,患者需要有可测量的疾病,Barcelona Clinic Liver Cancer(BCLC)分期B期或C期,ECOG表现状态为0或1,充足的器官和骨髓功能,以及Child-Pugh a级。如果在随机分组前28天以上,则允许既往切除、肿瘤消融、放疗或动脉化疗。
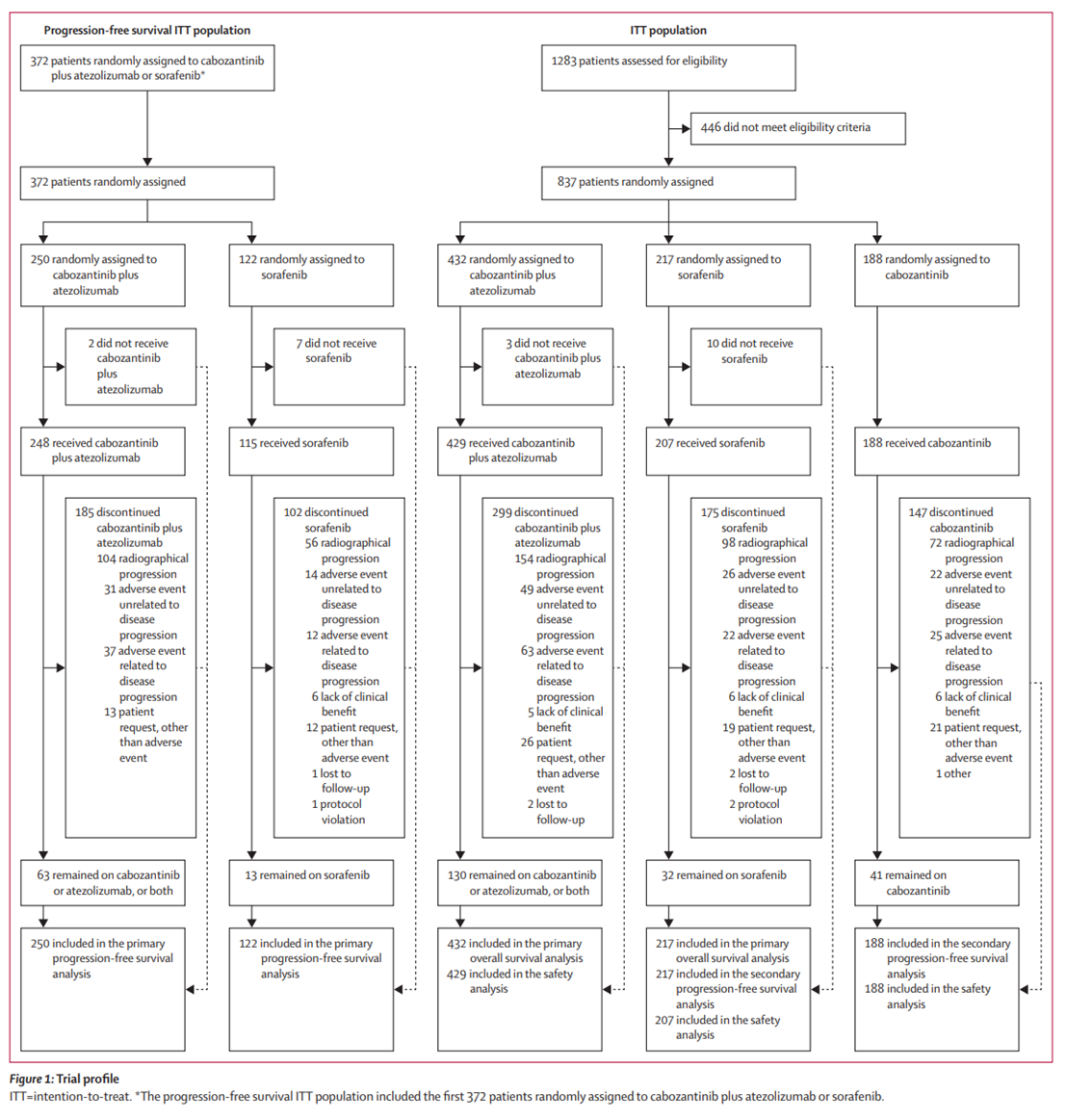
患者被随机分配(2:1:1)卡博替尼联合组(卡博替尼40mg口服、每日一次,加阿替利珠单抗1200mg静脉注射、每3周一次)、索拉非尼组(400mg口服、每日两次)或卡博替尼单药组(卡博替尼60mg口服,每日1次)。双重主要终点是随机分配给卡博替尼+阿替利珠单抗联合组或索拉非尼组的前372例患者(ITT人群)按照RECIST 1.1评估的无进展生存期,以及随机分配给卡博替尼+阿替利珠单抗联合组或索拉非尼组的总生存期(ITT人群)。此次分析报告了最终PFS和同期中期OS分析。
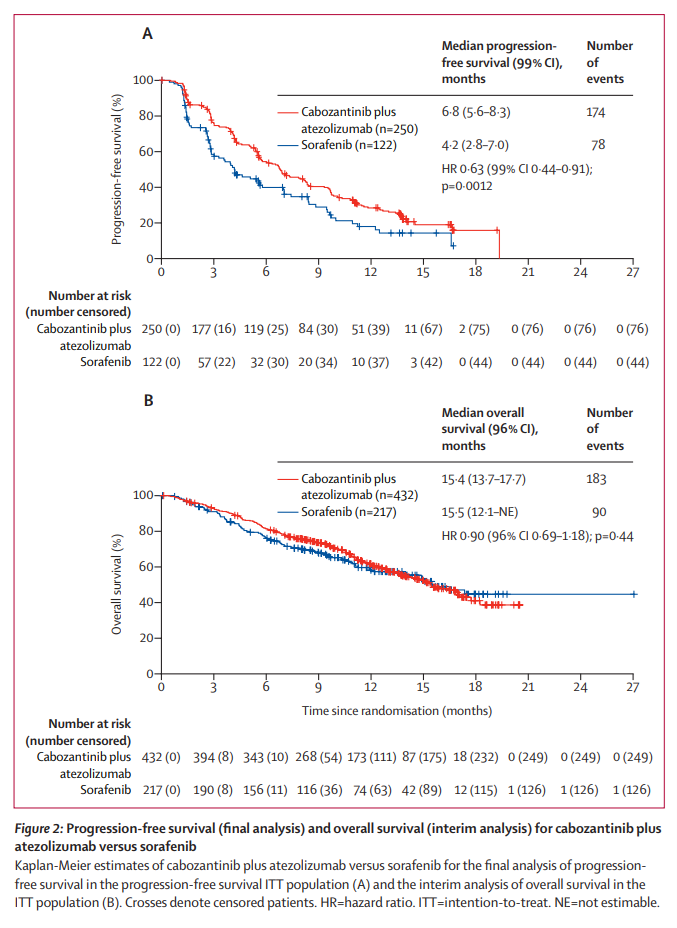
结果显示,数据截止时(2021年3月8日)的分析包括2018年12月7日至2020年8月27日期间随机分配的前837例患者,分别接受了卡博替尼+阿替利珠单抗联合治疗 (n=432)、索拉非尼(n=217)或卡博替尼单药 (n=188)治疗。ITT无进展生存人群的中位随访时间为15·8个月(IQR为14·5-17·2),ITT人群的中位随访时间为13·3个月(10·5-16·0)。联合治疗组中位PFS为6·8个月(99% CI 5·6 - 8·3),索拉非尼组中位PFS为4·2个月(2·8 - 7·0)( HR=0·63,99% CI 0·44-0·91,p=0·0012)。联合治疗组的中位OS(中期分析)为15.4个月(96% CI 13.7 - 17.7),而索拉非尼组的中位OS为15.5个月(12.1-不可估量)(HR 0.90, 96% CI 0.69 - 1.18;p = 0·44)。
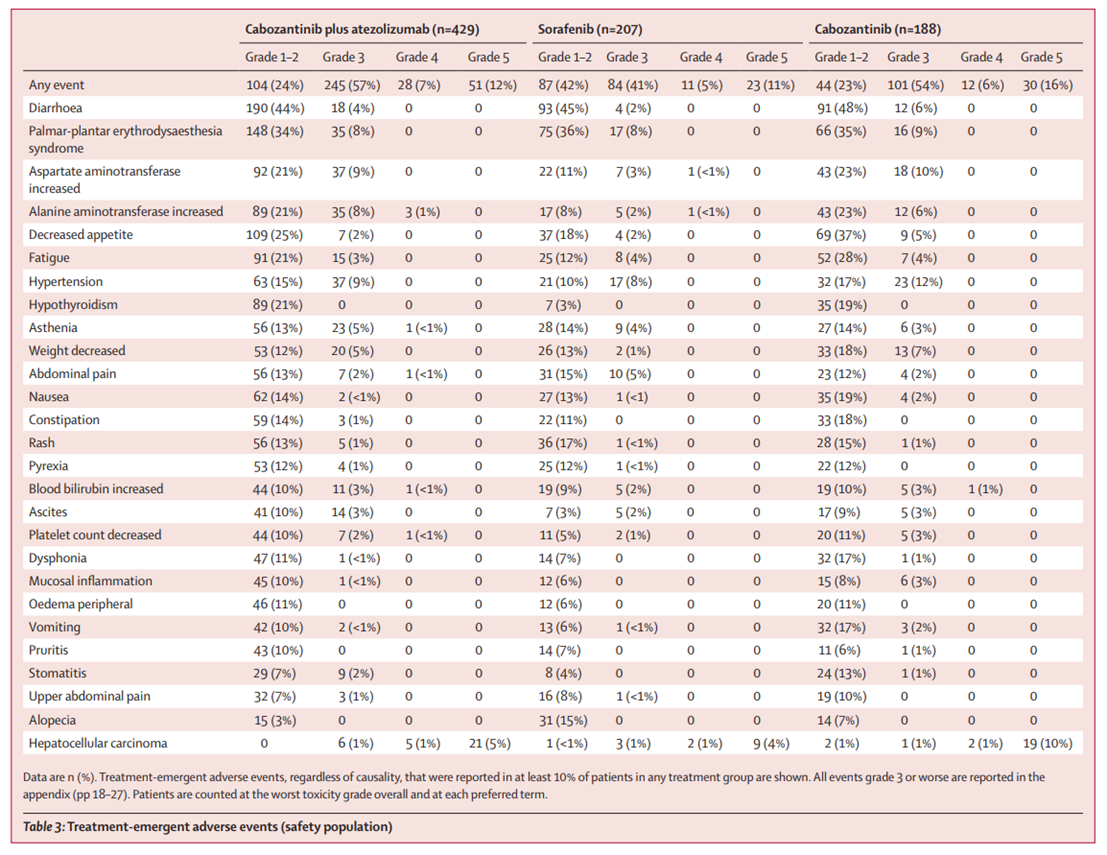
最常见的3或4级不良事件是丙氨酸转氨酶升高(联合治疗组429例患者中有38例[9%],索拉非尼组207例患者中有6例[3%],单药卡博替尼组188例中有12例[6%])、高血压(37例[9%]vs 17例[8%]vs 23例[12%])、天冬氨酸转氨酶升高(37例[9%]vs 8例[4%]vs 18例[10%])、以及手足综合征(35例[8%]vs 17例[8%]vs 16例[9%]);联合治疗组有78例(18%)患者,索拉非尼组有16例(8%)患者,单药卡博替尼组有24例(13%)患者发生严重的治疗相关不良事件。联合治疗组有6例(1%)患者发生治疗相关的5级事件(脑病、肝衰竭、药物性肝损伤、食管静脉曲张出血、多器官功能障碍综合征和肿瘤溶解综合征),索拉非尼组有1例(<1%)患者(全身健康状况恶化),单药卡博替尼组有1例(<1%)患者(胃肠道出血)。
在这项研究中,卡博替尼加阿替利珠单抗改善了无进展生存期,表明该组合为既往未通过全身性抗癌治疗的晚期肝细胞癌患者带来临床益处。但在总生存期方面缺乏益处,同时阿替利珠单抗联合贝伐珠单抗的可用性表明,需要进一步研究来确定卡博替尼加阿替利珠单抗是否为选定患者群体的一个适当的一线治疗方案。
原文来源:
Robin Kate Kelley , et al. Cabozantinib plus atezolizumab versus sorafenib for advanced hepatocellular carcinoma (COSMIC-312): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 2022 Published Online July 4, 2022 https://doi.org/10.1016/ S1470-2045(22)00383-7
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#I期临床#
91
#III#
93
#临床结果#
84
#替利珠单抗#
100
失败了
95
#肿瘤学#
67
#II期临床#
86
#III期#
83