Lancet:家族性高胆固醇血症注意了——胆固醇达标可以明显降低心血管危险!
2021-11-06 MedSci原创 MedSci原创
家族性高胆固醇血症的诊断很晚。威廉亚洲博彩公司 推荐的低密度脂蛋白胆固醇浓度不常通过单一药物治疗达到。
欧洲动脉硬化学会家族性高胆固醇血症研究合作组织(FHSC)的全球登记处通过协调和汇集多国数据为全球监测家族性高胆固醇血症提供了一个平台。在这项研究中,研究人员旨在描述杂合子家族性高胆固醇血症的成年人口的特征,并描述其在全球范围内的检测和管理。
研究人员利用FHSC全球注册数据,对临床或基因诊断为可能或明确的杂合子家族性高胆固醇血症的成人(18岁或以上)进行了横断面评估,当时他们被录入注册表。对数据进行了总体评估,并按世卫组织地区、性别以及指数病例与非指数病例进行了评估。结果发表在Lancet杂志上。
在登记的61612人中,来自56个国家的42167名成人(21999[53.6%]女性)被纳入研究。其中,31798人(75.4%)被诊断为荷兰脂质诊所网络标准,35490人(84.2%)来自欧洲的WHO地区。参与者进入登记册时的中位年龄为46.2岁(IQR 34.3-58.0);诊断为家族性高胆固醇血症时的中位年龄为44.4岁(32.5-56.5),其中40.2%的参与者在诊断时小于40岁。
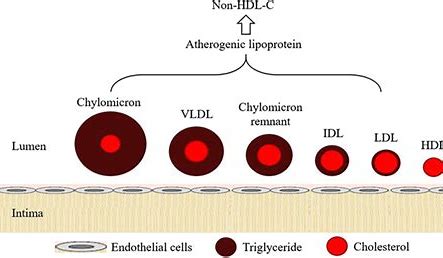
结果显示,心血管危险因素的流行率随着年龄的增长而逐渐增加,并因世卫组织地区而异。冠心病的发病率为17.4%(中风为2.1%,外周动脉疾病为5.2%),随着未经治疗的LDL-C浓度的增加而增加,女性比男性低约2倍。在接受降脂药物的患者中,16803人(81.1%)接受他汀类药物治疗,3691人(21.2%)接受联合治疗,男性比女性更多地使用更有效的降脂药物。
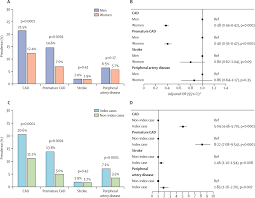
使用降脂药物治疗前后LDL-c的变化
在未服用降脂药物的患者中,LDL-C中位数为5.43 mmol/L(IQR 4.32-6.72),在服用降脂药物的患者中,中位数为4.23 mmol/L(3.20-5.66)。在服用降脂药物的患者中,2.7%的人的LDL-C低于1.8 mmol/L;使用联合治疗,特别是使用三种药物和PCSK-9抑制剂,与LDL-C低于1.8 mmol/L的比例和概率更高有关。与指数病例相比,非指数病例的患者更年轻,LDL-C更低,心血管危险因素和心血管疾病的发生率更低。
家族性高胆固醇血症的诊断很晚。威廉亚洲博彩公司 推荐的低密度脂蛋白胆固醇浓度不常通过单一药物治疗达到。
参考文献:
Global perspective of familial hypercholesterolaemia: a cross-sectional study from the EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). https://doi.org/10.1016/S0140-6736(21)01122-3
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言

















#Lancet#
52
学习一下
74
#高胆固醇血症#
76
#家族性#
50
#心血管危险#
67
不错不错
94