Nature Chem Bio:针对BCL-XL的高效小分子抑制剂WEHI-539被发现
2013-05-06 MedSci MedSci原创
日前,澳大利亚和美国Genentech公司的科学家合作,成功开发出了一种针对促存活蛋白BCL-XL的高效选择性小分子抑制剂。这项发现使开发针对BCL-XL的特定抗癌药物成为可能。BCL- XL属于一类有利于癌细胞存活的家族蛋白中的一种,其在肿瘤中通常过度表达。因为该蛋白家族很难作为小分子的标靶,所以只有一小部分药物能在临床发展应用 中有所表现。迄今为止,这些药物中没有一种能对特定的蛋白家族成员
日前,澳大利亚和美国Genentech公司的科学家合作,成功开发出了一种针对促存活蛋白BCL-XL的高效选择性小分子抑制剂。这项发现使开发针对BCL-XL的特定抗癌药物成为可能。
BCL- XL属于一类有利于癌细胞存活的家族蛋白中的一种,其在肿瘤中通常过度表达。因为该蛋白家族很难作为小分子的标靶,所以只有一小部分药物能在临床发展应用 中有所表现。迄今为止,这些药物中没有一种能对特定的蛋白家族成员产生选择性,而这个蛋白家族有可能引发一些williamhill asia 不愿意看到的毒性。
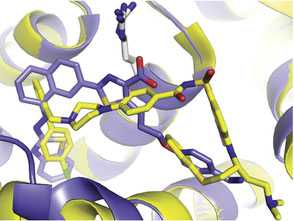
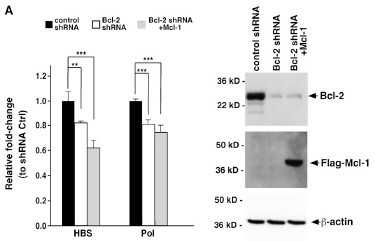
研究人 员设计了一种针对BCL-XL的高效选择性抑制剂。他们确认这种名为WEHI-539的化合物在细胞中具有高效率和选择性的特点,并且能作用于标靶,促进细胞凋亡。科学家可将WEHI-539作为一种重要的工具以更好地了解BCL-XL与癌细胞之间的关系,并为开发针对BCL-XL的特定抗癌药物开启了一 扇大门。
原始出处:
Guillaume Lessene, Peter E Czabotar, Keith G Watson et al. Structure-guided design of a selective BCL-XLinhibitor. Nature Chemical Biology, 21 April 2013; doi:10.1038/nchembio.1246
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#Nat#
43
#小分子抑制剂#
63
#小分子#
52
#抑制剂#
38
#Bio#
42
#Bcl-xL#
57