新一代降脂单抗药PCSK9呼之欲出
2015-06-18 孙学军 科学网博文
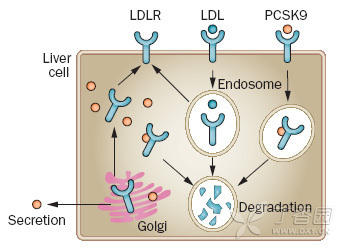
高胆固醇血症是冠心病的风险因子,其特征为高血浆低密度脂蛋白胆固醇水平。最常见见生物分子原因有2个,一是低密度脂蛋白受体基因突变,二是低密度脂蛋白受体的配体蛋白apoB的功能缺陷。2003年法国学者又发现第3个导致高胆固醇血症关键基因,就是蛋白转化酶枯草杆菌蛋白酶/西布曲明9a型(PCSK9)。经典的降血脂药物他汀类药物,也是目前临床上广泛使用,并取得理想治疗效果的药物,其关键作用是通过阻断体内
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#单抗药#
42
#呼之欲出#
52
#PCS#
52
#Csk#
50
看看
148
希望早点应用
124
挺好的。
182
好友想法
130
厉害
95
有见解
86