我国《CAR-T细胞制剂制备质量管理规范》征求意见稿发布
2018-05-04 佚名 医谷
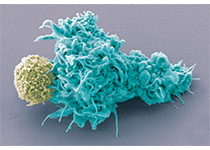
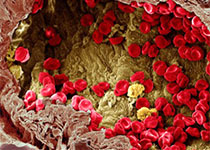
近年来,免疫治疗经历了一系列突飞猛进的发展,以特异性过继免疫细胞疗法及免疫检查点抗体疗法为代表的新型免疫治疗技术因其在临床研究中取得的显着疗效而成为学术界和产业界共同关注的焦点。其中,嵌合抗原受体T细胞免疫疗法(Chimeric Antigen Receptor T-Cell Immunotherapy,CAR-T疗法)因其在白血病、淋巴瘤、多发性骨髓瘤的治疗中展现出显着的治疗效果而成为国内外

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#CAR-#
50
#管理规范#
59
#征求意见稿#
55
#征求意见#
40
#质量管理规范#
49
#质量管理#
73
了解一下谢谢
70
学习了.谢谢分享
98
近年来.免疫治疗经历了一系列突飞猛进的发展.以特异性过继免疫细胞疗法及免疫检查点抗体疗法为代表的新型免疫治疗技术因其在临床研究中取得的显着疗效而成为学术界和产业界共同关注的焦点.其中.嵌合抗原受体T细胞免疫疗法(ChimericAntigenReceptorT-CellImmunotherapy.CAR-T疗法)因其在白血病.淋巴瘤.多发性骨髓瘤的治疗中展现出显着的治疗效果而成为国内外研究的热点
104