罕见鞍区孤立性梭形细胞肉瘤样癌一例
2019-06-18 周迎 袁涛 刘小海 中国医学科学院学报
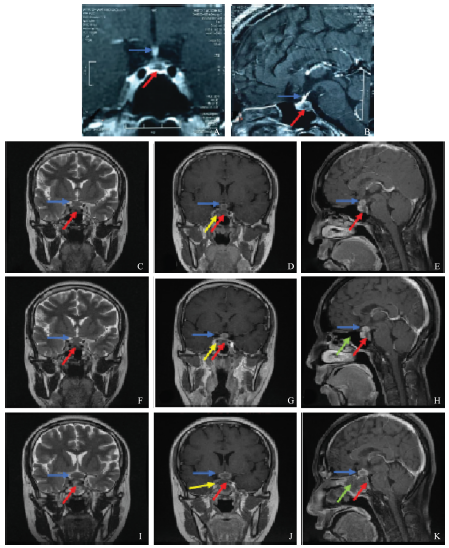
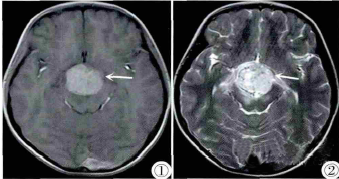
患者,女,33岁,因“头痛、多尿、多饮8月,月经紊乱3月,视力下降1周”入院。患者于2015年1月无明显诱因出现多尿、多饮,饮水量10L/d,饮水量与尿量相当,伴双颞侧间断性头部胀痛,就诊于当地医院行头部MRI,提示鞍内占位(大小约12mm×6mm×13mm),垂体柄增粗,未诊治。6月尿量减少至3L/d,同时出现月经紊乱,未予重视。9月出现视力下降(<10 cm),遂至北京协和医院内分泌科门诊就诊

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#梭形细胞#
0
好
115
#罕见#
62
#鞍区#
55
#孤立性#
46
学习
75
非常少见,感谢分享。
104
#肉瘤样癌#
69