Neurology:小儿卒中年龄是远期认知预后关键,幼年卒中(29天-6岁)影响极大
2022-01-06 Naomi MedSci原创
儿童缺血性卒中是一种罕见的事件,但伴随着认知和神经后遗症风险的增加。卒中年龄是卒中预后的一个重要因素,并影响长期认知结果,与病变大小和病变位置无关。儿童早期卒中后,儿童长期认知功能改变的风险极大
儿童动脉缺血性卒中是一种罕见的事件,但伴随着认知和神经后遗症风险的增加。多年来,与不良预后相关的因素的识别一直是研究的重点;然而,关于预后预测的研究仍然不足。
由于在此期间快速的突触发生以及神经元网络髓鞘形成和重组过程的增加,建议发育中的大脑在早期脑损伤后更灵活,恢复能力更好。另一方面,发育中的大脑特别容易受到早期的脑损伤,导致大脑发育中断。鉴于可塑性和易损性这两种相互矛盾的观点,关于年龄对儿童中风影响的研究结果仍不清楚,一些研究还没有明确的结论。由于在这一时期快速的突触发生以及神经元网络的髓鞘形成和重组过程,发育中的大脑在早期脑损伤后的恢复能力更强。另一方面,发育中的大脑特别容易受到早期的脑损伤,导致大脑发育中断。
虽然有几项研究检测了急性期直到卒中后两年的认知结果,但研究调查慢性晚期(卒中后>2年)患者的结果是有限的。关注慢性晚期的患者是至关重要的,因为随着时间的推移,缺陷可能会出现并增加康复过程可能远远超过中风后的最初几个月。此外,脑损伤时的发展阶段可以调节认知结果。认知发展的关键时期内的脑侮辱可能导致比认知功能出现之前或之后发生的脑损伤更差的认知结果。此外,认知功能,特别是执行功能,与生活质量、学业成就、社交能力,这强调了监测卒中后认知结果的重要性。近日,有研究学者检查了慢性期(卒中后2年以上)儿童卒中后的长期认知结果,并调查年龄是否在卒中对认知的影响,以确定认知结果较差的患者的风险。
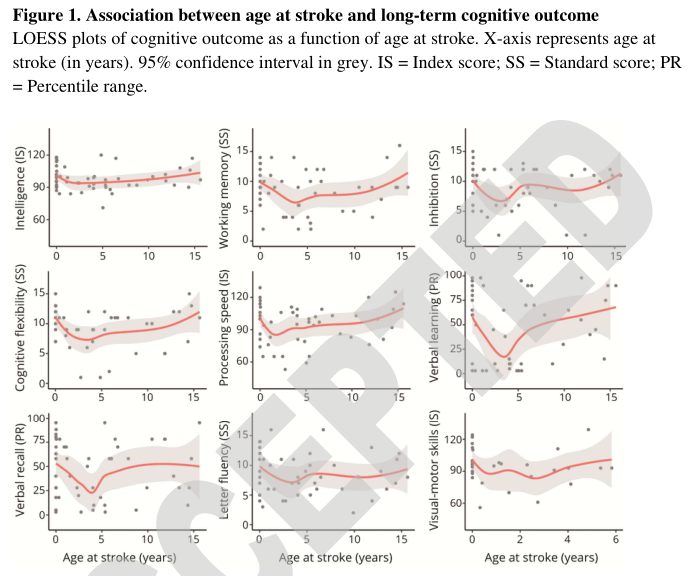
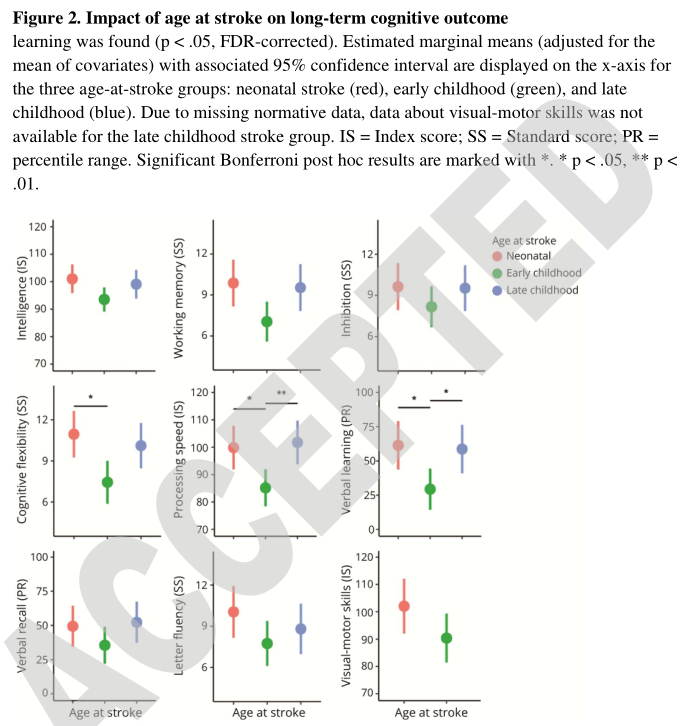
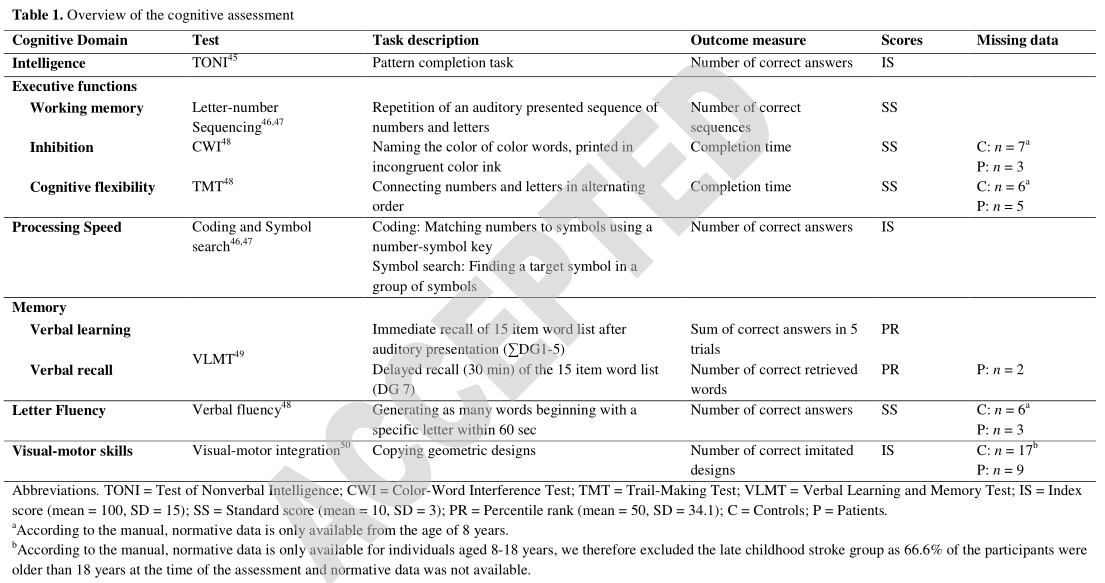
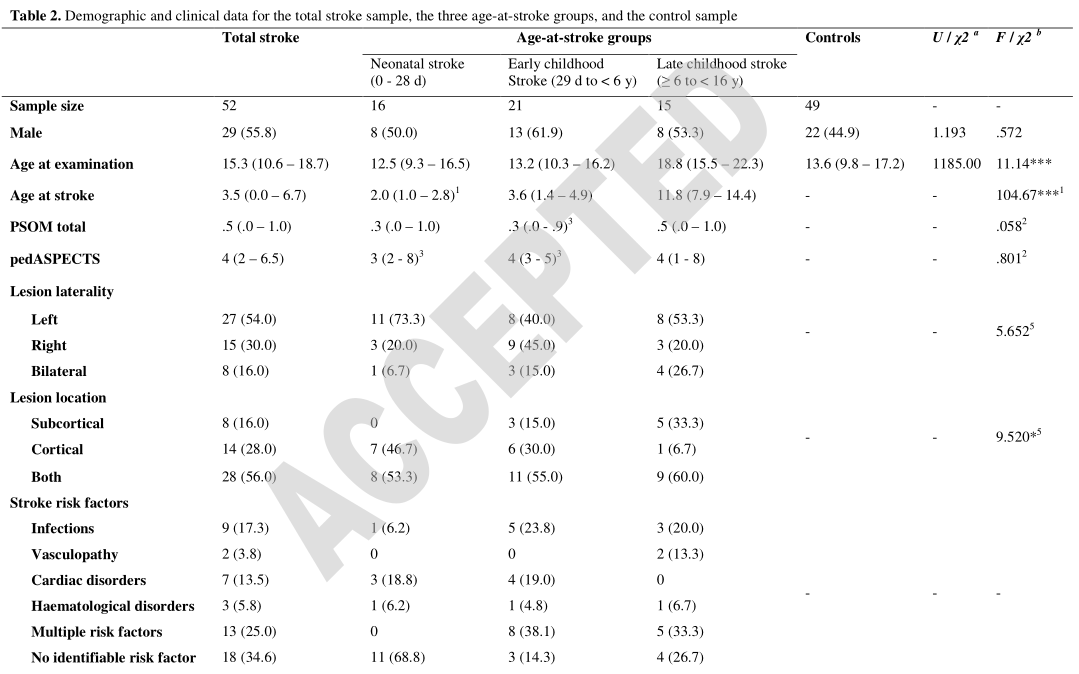
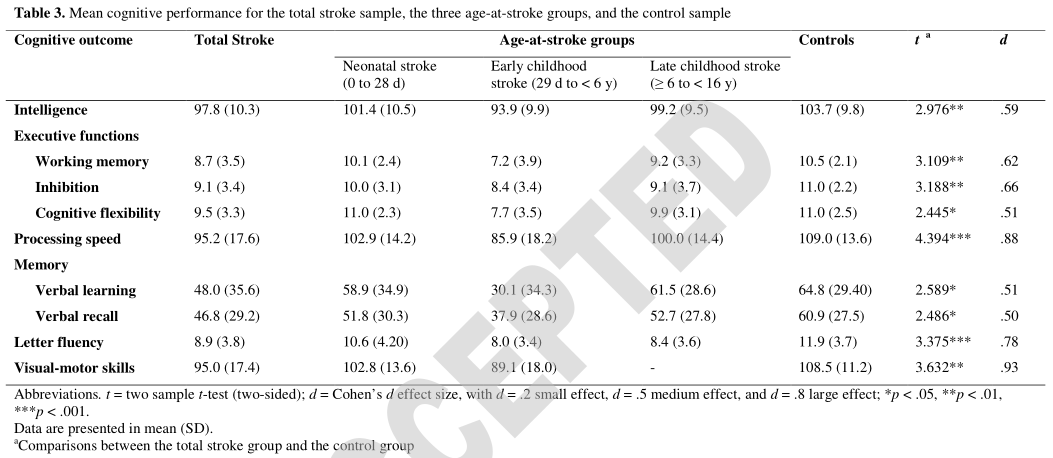
这项横断面研究包括先前诊断为新生儿或儿童动脉缺血性中风的中风慢性期患者(中风后2年以上)和对照组。患有活动性癫痫、严重学习困难或行为问题阻碍认知评估的参与者被排除在外。通过神经心理学测试评估了几个认知领域,包括智力、执行功能(工作记忆、抑制和认知灵活性)、处理速度、记忆、字母流畅性和视觉运动技能。对新生儿卒中(出生0至28天的中风)、儿童早期卒中(卒中29天至<6岁)和儿童晚期卒中(≥6至<16岁的中风)患者的认知长期结果进行比较。
- 52例新生儿或儿童动脉缺血性卒中患者(中位年龄:15.3岁,IQR=10.6~18.7)和49例健康对照组(中位年龄:13.6岁,IQR=9.8~17.2)符合纳入标准。
- 与对照组相比,儿童卒中组的认知结果明显更差。
- 中风时年龄(与病灶大小和部位无关)对认知灵活性、处理速度和语言学习的非线性影响在早期儿童卒中(29天至<6岁)中显示出显著的意义。与新生儿、儿童晚期卒中相比,认知结果更差(p<0.05,FDR已更正)。
卒中年龄是卒中后恢复的一个重要因素,并影响长期认知结果,与病变大小和病变位置无关。儿童早期发生卒中,长期认知功能改变的风险极大。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














好文章,前几天刚遇到一例患者
62
学习了
86
学习了
93
#Neurol#
73
好文章啊!
99
感谢分享,学习了
95
非常不错
123
小儿卒中的发病
0
学习了
90
认真学习了
57