BMJ Open:不同剂量普卡洛必利治疗慢性特发性便秘研究
2021-02-16 MedSci原创 MedSci原创
每个人都曾有过有一种叫做便秘的“难言之隐”。而慢性特发性便秘(CIC)指的是持续性的、且无法从生理结构或者生物化学等方面解释的便秘。据数据显示,全球成年人CIC患病率约为14%
每个人都曾有过有一种叫做便秘的“难言之隐”。而慢性特发性便秘(CIC)指的是持续性的、且无法从生理结构或者生物化学等方面解释的便秘。据数据显示,全球成年人CIC患病率约为14%,年龄在65岁以上,女性可能是患病率上升的潜在危险因素。
对于胃肠道医生和外科医生来说,对CIC管理面临着艰巨的挑战,尽管缓泻剂和促动力剂治疗CIC已广泛用于临床实践,但临床上长期疗效的证据仍然不足。此外,肠胃蠕动减弱和肠神经系统(INS)的受损明显促进CIC的发生。因此,建议对CIC进行合理的治疗应集中在INS中的神经元上,进而改善CIC。
近日,发表在BMJ Open杂志的一项研究显示,无论使用1mg,2mg或4mg剂量,普鲁卡必利均可有效治疗CIC患者。

在这项研究中,研究人员全面检索PubMed,EMBASE,MEDLINE以及Cochrane等数据库,选择了不同剂量的普考洛必利的前瞻性试验。首次在荟萃分析中综合了每周的自发排便频率(SBM)和突发性治疗不良事件(TEAE),例如头痛,心律不齐,腹泻,头晕,恶心和呕吐。然后,通过贝叶斯分析对普卡洛必利最佳剂量的可能性进行排序。
结果显示,在对14项针对4328例患者高质量随机对照试验(RCT)分析显示,使用1mg(OR:2.40,95%CI 1.32~4.37)、2mg(OR:2.55,95%CI 1.93~3.36)和4mg(OR:2.51,95%CI 1.92~3.28)普鲁卡必利后,SBMs显著增加。贝叶斯分析表明,与2mg和4mg剂量相比,使用1mg剂量的普鲁卡必利的SBMs显著提高(OR:3.31,95%可信区间1.72至6.16,概率等级=0.70)。
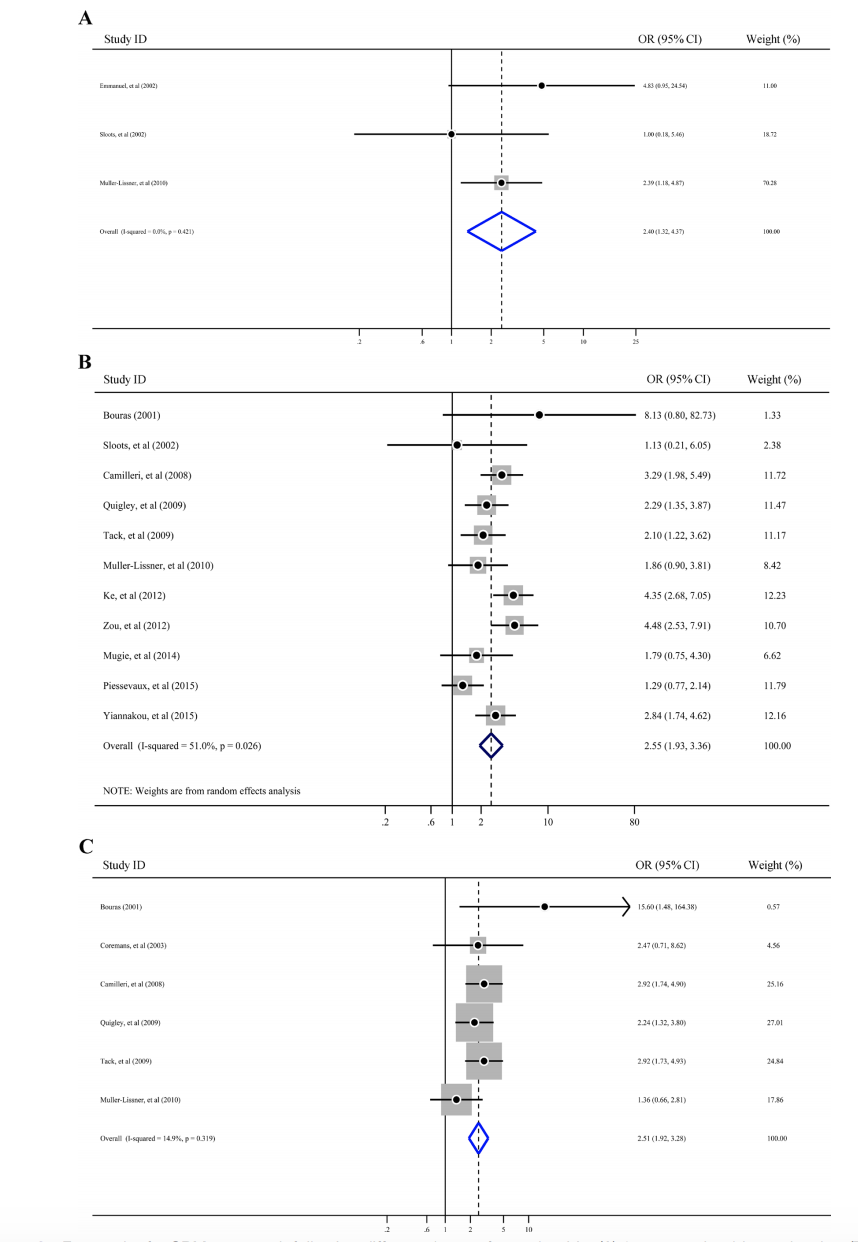
不同剂量普鲁卡必利SBMs的森林图
然而,在TEAEs方面,使用2mg(风险比(RR):1.20,95%CI 1.09至1.33)和4mg(RR:1.14,95%CI 1.07至1.22)普鲁卡必利的TEAEs明显更高,而1mg剂量未达到统计学意义(RR:1.17,95% CI 0.94至1.44)。
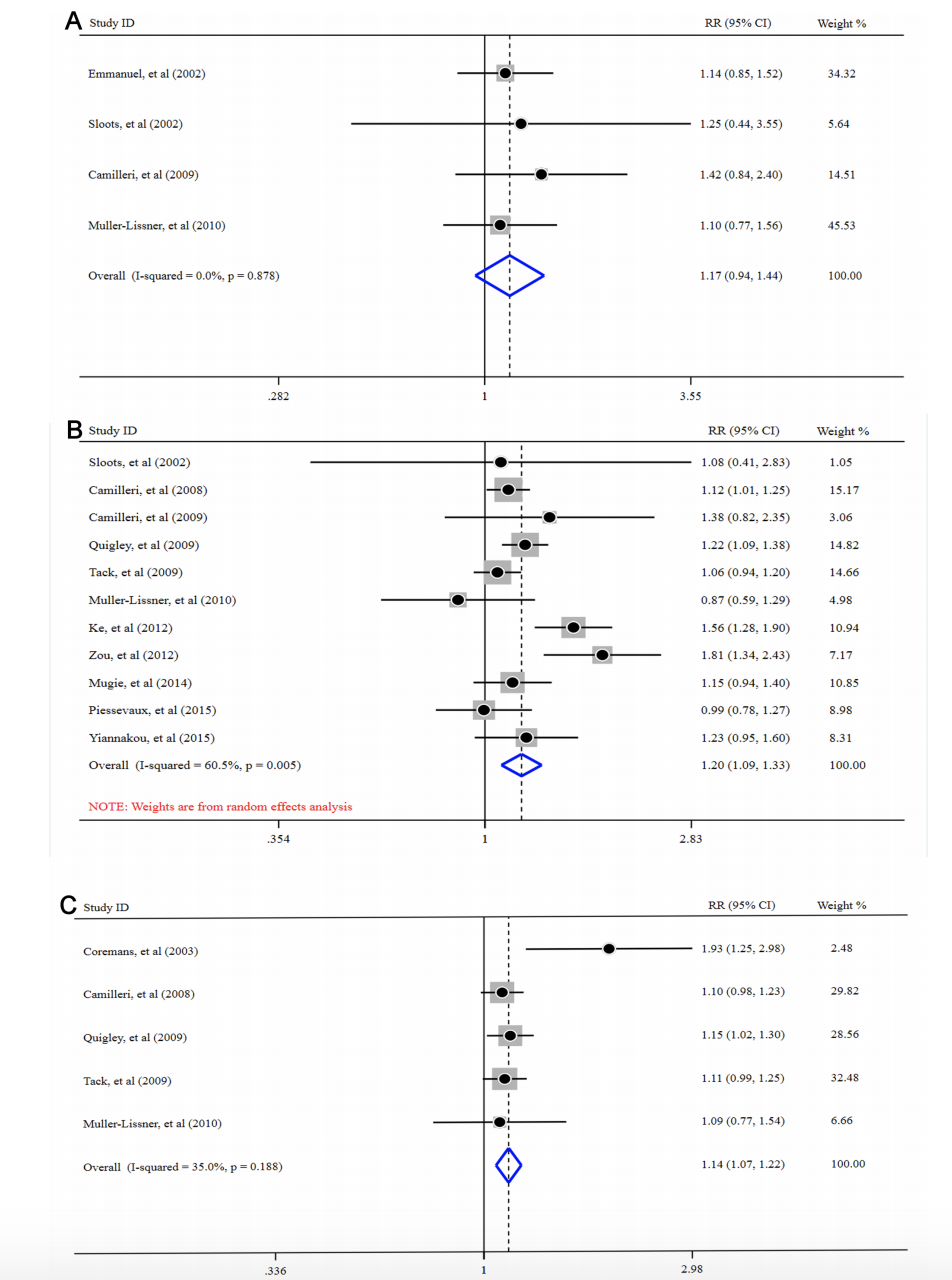
不同剂量普鲁卡必利的TEAEs森林图
总之,使用1mg剂量普鲁卡必利可以有效治疗CIC,而该研究存在一定的局限性。众所周知,CIC是一种肠功能障碍的慢性疾病,需要长期用药,因此需要更多的更大范围的RCT和长期的疗效评估来平衡普卡洛必利在CIC治疗中的风险效益。
原始出处
Tao Yang, Kaili Wang et al.Different doses of prucalopride in treating chronic idiopathic constipation: a meta-analysis and Bayesian analysis.BMJ Open 2021;11:e039461. doi:10.1136/ bmjopen-2020-039461
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#BMJ#
115
#PE#
57
#特发性#
69
Bu学习
96
#便秘#
0
表示很关注这个话题
100
学习不同领域的新内容了
106