JAHA:房颤患者缺血性卒中严重程度和死亡率的关系
2022-02-14 MedSci原创 MedSci原创
在当代全国缺血性卒中患者队列中,与非AF患者相比,AF患者的卒中更严重,死亡率更高。死亡率的差异主要由卒中严重程度所介导。
缺血性卒中是心房颤动(AF)患者的主要风险,是患者风险分层和考虑抗凝治疗的基础。这是恢复的最重要因素之一。AF估计占所有缺血性卒中的20%至25%。

目前,缺乏AF患者卒中严重程度和预后的当代数据。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员的目标是调查患有和不患有心房颤动(AF)的患者的卒中严重程度和随后的死亡率。
丹麦卒中登记处(2005年1月至2016年12月)的首次缺血性卒中患者被纳入一项观察性研究。房颤患者与无房颤患者按性别、年龄、年份和CHA2DS2-VASc评分1:1进行匹配。卒中严重程度由斯堪的纳维亚卒中量表(0-58分)来衡量。研究人员通过Kaplan-Meier和多变量Cox回归估计死亡率。
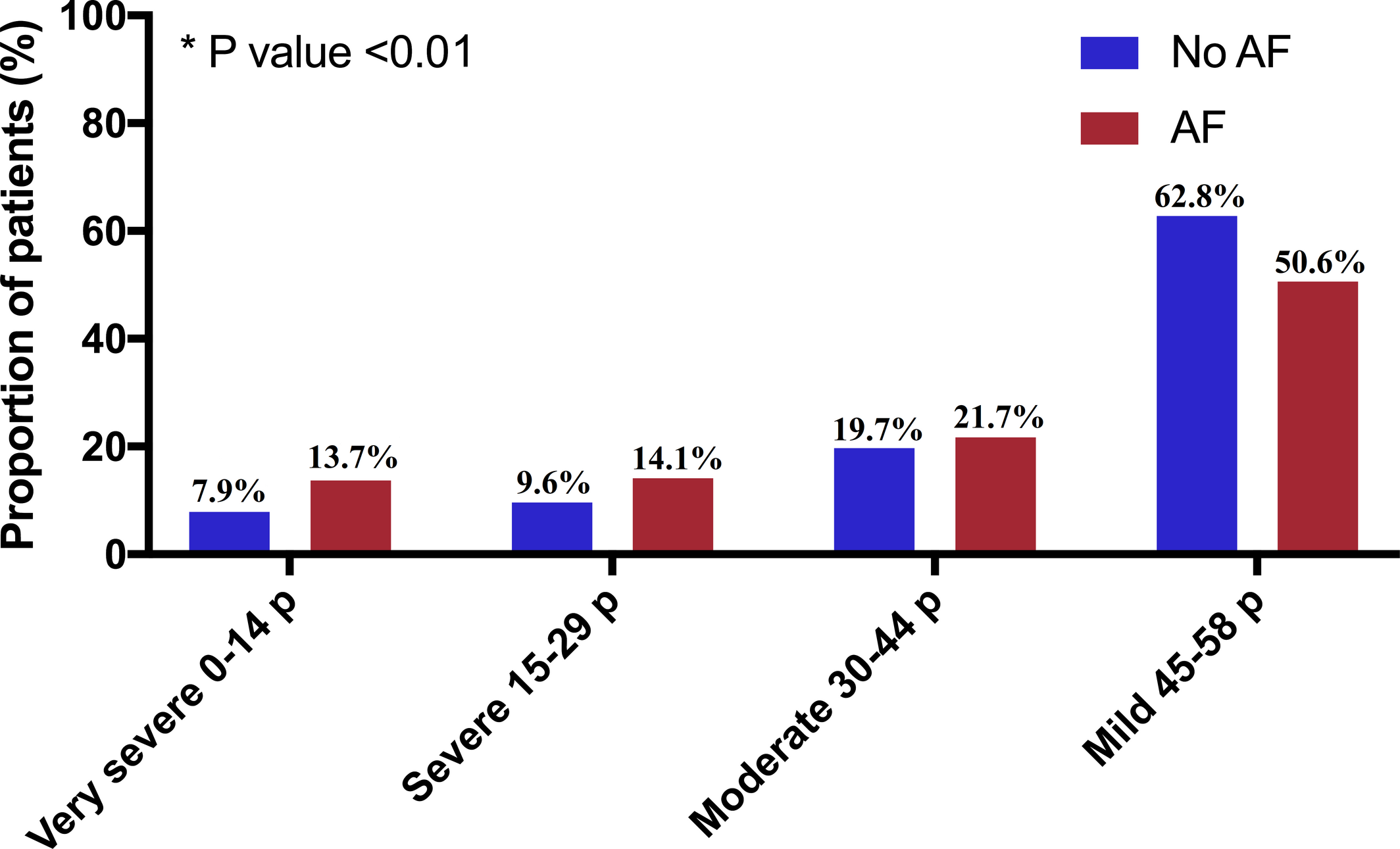
在86458名已确定的卒中患者中,17205名患有AF。匹配后,研究人员纳入了14662名AF患者和14662名无AF患者(51.8%的女性;中位年龄为79.6岁[第25-75个百分位为71.8-86.0])。与没有AF的患者相比,更多的AF患者发生非常严重的卒中(0-14分)(13.7% vs. 7.9%,P<0.01)。AF患者30天和1年死亡率的绝对发生率(分别为12.1%和28.4%)明显高于无AF患者(分别为8.7%和21.8%)。这在调整后的30天死亡率模型中,这一结果也成立(风险比[HR]为1.40[95%CI为1.30-1.51])。然而,当额外调整卒中严重程度时,这种关联变得不显著(HR为1.10[95%CI为1.00-1.23])。AF与较高的1年死亡率相关(HR为1.39[95%CI为1.32-1.46]),尽管它是由卒中严重程度所介导(HR为1.15[95%CI为1.09-1.23],模型包含卒中严重程度)。
由此可见,在当代全国缺血性卒中患者队列中,与非AF患者相比,AF患者的卒中更严重,死亡率更高。死亡率的差异主要由卒中严重程度所介导。
原始出处:
Naja E. Vinding.et al.Ischemic Stroke Severity and Mortality in Patients With and Without Atrial Fibrillation.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.022638
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#缺血性卒#
0
#缺血性#
81
#AHA#
58
#房颤患者#
88