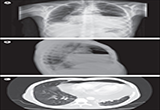
Lancet:常规插管后的张力性水气心包
2015-05-04 MedSci MedSci原创
2014年6月,一个患有晚期肾病和慢性尿毒症心包积液的37岁病人来到williamhill asia 机构,伴随逐渐恶化的呼吸困难和端坐呼吸,肾切除手术4天后控制高血压。他在拒绝移植肾的前9年每周3次定期进行血液透析。检查静息时病人出现严重呼吸困难,脉搏102次每分钟,呼吸率20次每分钟,血压110/70 mm Hg,伴有25mm Hg诡异变化。肺听诊显示基部支气管呼吸声。胸部X线表明有气-液水平的心脏肥大。胸部CT显示心包积

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








特殊病例学习了。
122
#Lancet#
54
#张力#
45