Chin J Cancer Res:阿帕替尼单药或联合治疗HER2阴性乳腺癌伴有胸壁转移患者的疗效:多中心II期临床研究
2021-12-23 yd2015 MedSci原创
研究表明,阿帕替尼治疗乳腺癌合并CWM疗效显著,尤其是与内分泌联合治疗。未接受胸壁放疗的HR+患者PFS显著改善。然而,不良反应也是比较明显的,需要密切监测。
研究表明,乳腺癌(BC)伴胸壁转移(CWM)常表现为丰富的新生血管。提示抗血管治疗对该类型患者可能起到较好疗效。因此,来自北京大学等多个中心团队开展了一项多中心II期临床研究,探讨了阿帕替尼治疗HER2阴性乳腺癌伴有CWM患者的疗效和安全性。相关研究结果 Chinese Journal of Cancer Research杂志上。
该研究是2016年9月到2020年3月期间在中国的四个中心进行。患者接受500 mg/d的阿帕替尼(如果激素受体阳性(HR+),可单独或与内分泌治疗),直到疾病进展或不可接受的毒性。无进展生存期(PFS)是主要终点。
在2016年9月至2019年7月期间,30名患者被纳入该研究,最后一次随访日期为2020年3月30日。中位年龄49.5岁(35 ~ 69岁),HR+ 20例(66.7%)。除CWM外,最常见的转移部位为淋巴结、肺、骨和肝脏;17例(56.7%)患者有两个以上的转移部位。20例(66.7%)患者接受多线内分泌治疗。在可评估的26例患者中,仅CWM的患者(4.9个月)与同时伴有其他转移部位的患者(4.3个月)之间mPFS无显著差异(P=0.258)。
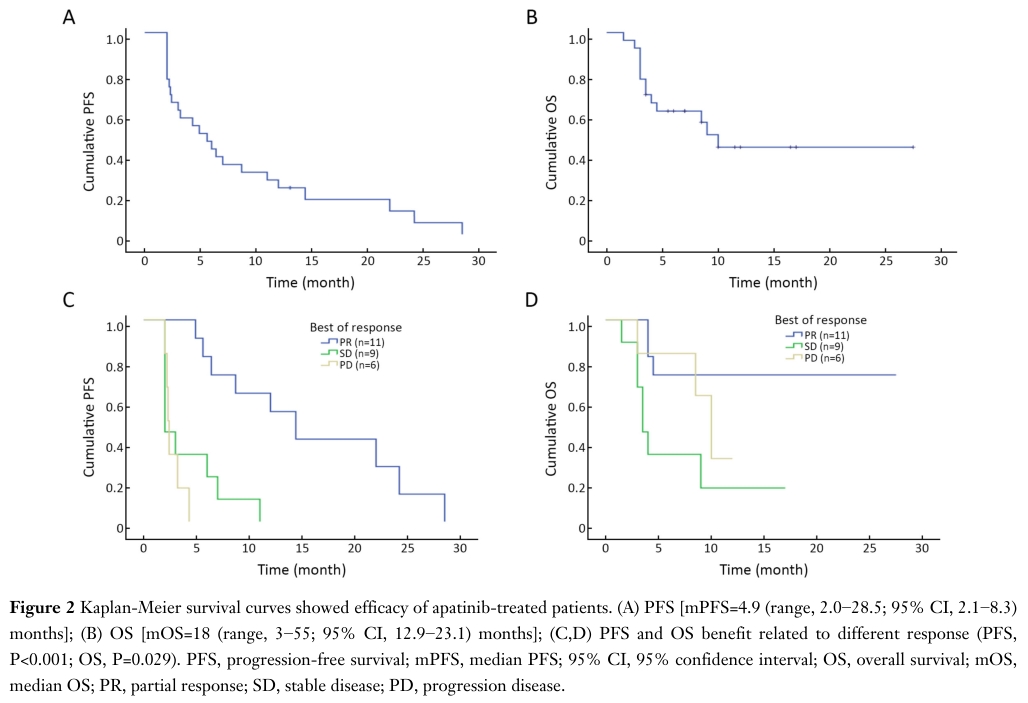
对26例患者进行疗效评价。中位无进展生存期(mPFS)和中位总生存期(mOS)分别为4.9[95%CI: 2.1 8.3)个月和18个月(95%CI:12.9-23.1)。在获得PR、SD和PD的患者中,mPFS分别为14.4、2.0和2.3个月(P<0.001);mOS分别为未达到,7个月和20个月(P=0.029)。
预后
客观有效率(ORR)为42.3%(11/26),疾病控制率(DCR)为76.9%(20/26)。

疗效评估
在亚组分析中,与TNBC(阿帕替尼单药治疗)患者相比,HR+患者(阿帕替尼联合内分泌治疗)的生存率显著提高;mPFS分别为7.0 个月(95% CI: 2.2 - 11.8)和2.3个月(95% CI: 1.2 - 3.4)(P=0.001)。在没有接受胸壁放疗的患者中mPFS为6.4个月(95% CI: 1.6 - 19.5),高于接受过胸壁放疗患者的3.0个月(95% CI: 1.3 - 4.6) (P=0.041)。术后有无淋巴结转移,转移部位以及数量等方面比较预后没有统计学差异。

亚组分析预后
在多因素分析中,HR+状态是有利PFS的唯一独立预测因素(P=0.014)。较长的OS仅与HR+状态和CWM相关(P=0.042和P=0.031)。
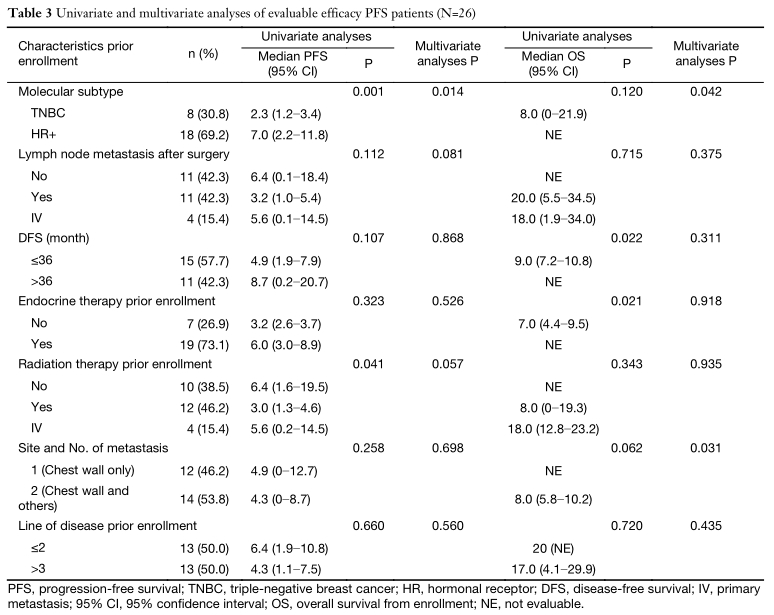
多因素分析
阿帕替尼药物相关不良事件发生率,1级为50.0%,2级为66.7%,3级为40.0%。
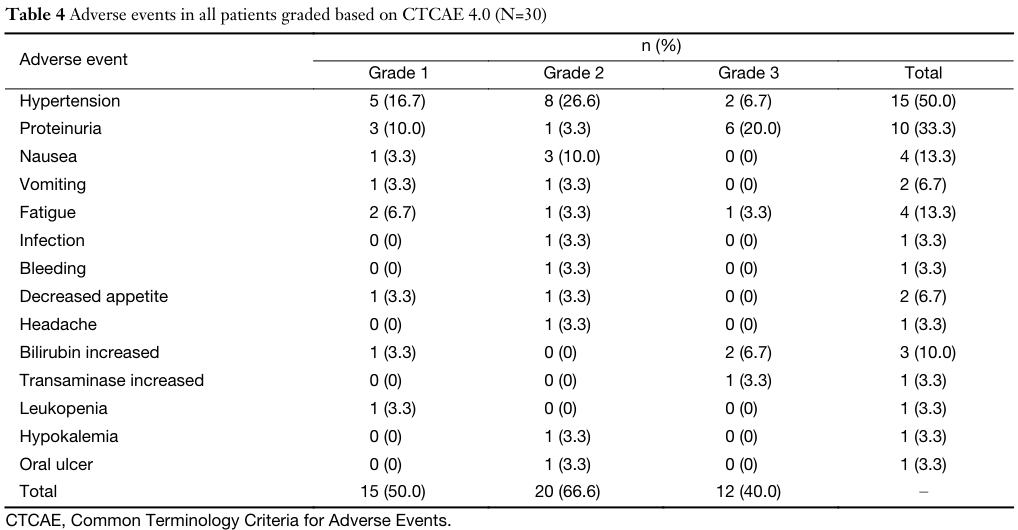
AEs
综上,研究表明,阿帕替尼治疗乳腺癌合并CWM疗效显著,尤其是与内分泌联合治疗。未接受胸壁放疗的HR+患者PFS显著改善。然而,不良反应也是比较明显的,需要密切监测。
原始出处:
Li H, Geng C, Zhao H, Jiang H, Song G, Zhang J, Liu Y, Gui X, Wang J, Li K, Tong Z, Zhao F, Yang J, Chen G, Liu Q, Liang X. Multicenter phase II study of apatinib single or combination therapy in HER2-negative breast cancer involving chest wall metastasis. Chin J Cancer Res. 2021 Apr 30;33(2):243-255. doi: 10.21147/j.issn.1000-9604.2021.02.11. PMID: 34158743; PMCID: PMC8181870.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#II期临床研究#
74
#I期临床#
68
#多中心#
77
#阴性乳腺癌#
75
#HER2阴性乳腺癌#
73
#联合治疗#
57
#HER2阴性#
69
#II期临床#
73