经皮肺动脉瓣植入术(PPVI)已成为先天性心脏病(CHD)治疗常规手术,并逐渐替代开胸手术。由于材料的使用寿命有限,这些患者经常发生右心室流出道功能障碍。用人工瓣膜重建右心室流出道的外科肺动脉瓣置换术(SPVR)或PPVI会增加感染性心内膜炎(IE)的风险。先天性心脏病肺瓣膜置换术后发生感染性心内膜炎(IE)是一个重要的临床问题。
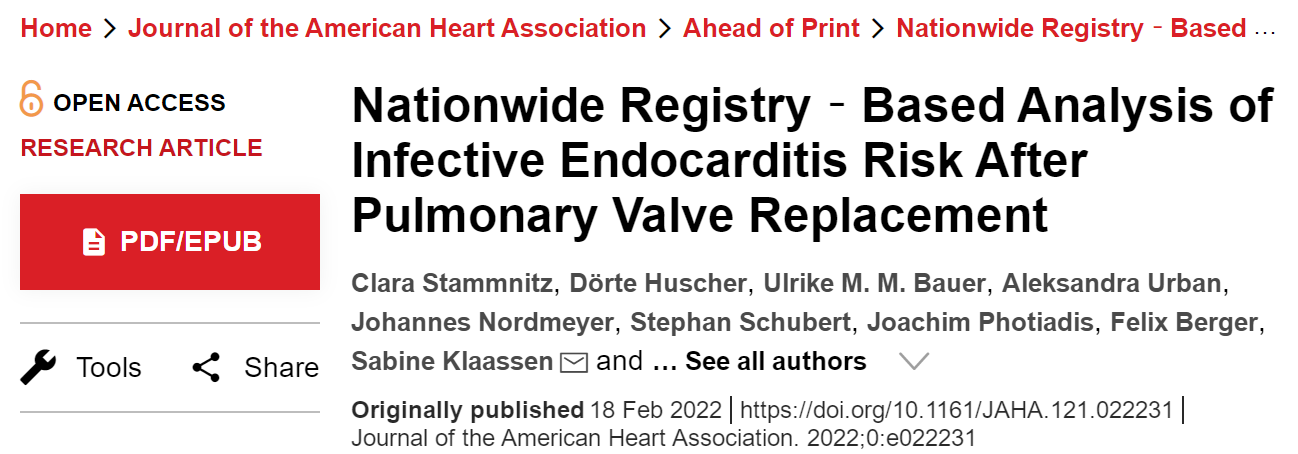
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在明确经皮肺动脉瓣植入或手术肺瓣膜置换术后IE的特定长期危险因素。
所有在2018年1月之前接受过至少1次肺动脉瓣置换术的国家先天性心脏缺陷登记处收录的先天性心脏病患者都被纳入研究。该研究共有1170名患者(56.3%为男性,研究纳入时的中位年龄为12岁[四分位距{Q1-Q3}为5-20岁])接受了1598次肺动脉瓣置换术。
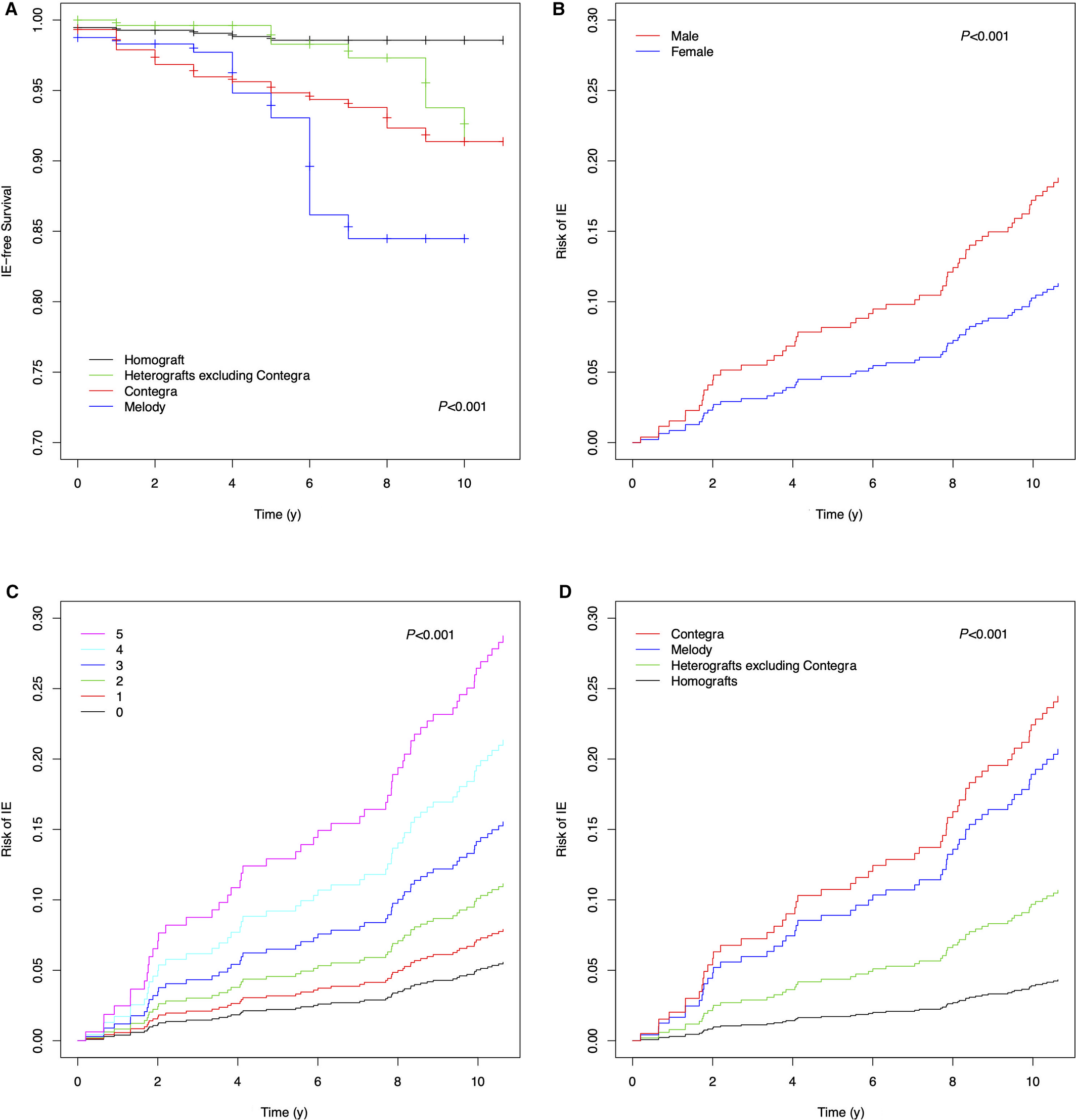
在总共9397人次每年的随访期间,4.8%的患者发生IE(中位数为10[Q1-Q3为6-10])。同种异体移植的558名(1.3%)患者中有7名发生IE,异种移植的723名(4.3%)患者中有31名和Melody瓣膜移植的241名(7.5%)患者中18名发生IE。Edwards Sapien和机械瓣膜的使用频率较低,并且仍然未发生IE。排除Contegra瓣膜的异种移植物患者中IE的发生率为278例有7例(2.5%),而纳入Contegra瓣膜的患者IE的发生率为445例中有24例(5.4%)。如果从异种移植物患者中排除Contegra瓣膜的个体,则与同种移植物相比,IE的风险没有增加(风险比[HR]为2.60;P=0.075)。牛颈静脉瓣膜、Contegra瓣膜(HR为6.72;P<0.001)和Melody瓣膜(HR为5.49;P<0.001)的IE风险增加,但Melody瓣膜和Contegra瓣膜(HR为1.01;P=0.978)则没有差异。
由此可见,牛颈静脉瓣膜具有最高的IE风险,无论手术方式如何。
原始出处:
Clara Stammnitz.et al.Nationwide Registry‐Based Analysis of Infective Endocarditis Risk After Pulmonary Valve Replacement.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.022231
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#置换#
67
#肺动脉瓣#
69
#肺动脉瓣置换#
0
#感染性#
86
#内膜#
60
#AHA#
46
#心内膜炎#
75
#置换术#
52