Biomed Pharmacother:黄芩苷和黄芩素对肺动脉高压的作用机制和治疗前景
2022-07-20 August MedSci原创
肺动脉高压(PH)是一种慢性致死性疾病,迫切需要新的治疗药物和方法。黄芩素和黄芩苷是中药黄芩的活性成分,具有广泛的药理活性。大量涉及 PH 体外和体内模型的研究表明,黄芩苷和黄芩素治疗可能是有效的。
肺动脉高压(PH)是一种神秘的分子起源的心血管疾病,涉及许多信号通路和病理变化,包括肺血管收缩、重塑和原位血栓形成,导致血管阻力增加和进行性肺动脉压(PAP)。PH特点是涉及肺小动脉收缩并伴有血管壁增生和重塑的复杂病理过程。现有的PH临床药物主要包括血管扩张剂,这些药物在阻止PASMCs增殖方面部分有效,但最终未能阻止肺血管重构过程。因此,迫切需要开发通过新机制发挥作用的 PH 药物。此文一直在对天然产物中用于治疗 PH 的新型化合物进行深入分析。根据发现,葛根素、丹酚酸 A、白藜芦醇和染料木素可通过不同于现有疗法的机制延缓 PH 的病理进展。
同样引人注目的是黄芩苷和黄芩素,天然黄酮类化合物,具有广泛的药理作用,包括抗炎、抗增殖和抗氧化,并提供内皮和心脏保护。最近,发现黄芩素在体外和体内都能抑制 SARS-CoV-2 引起的损伤。
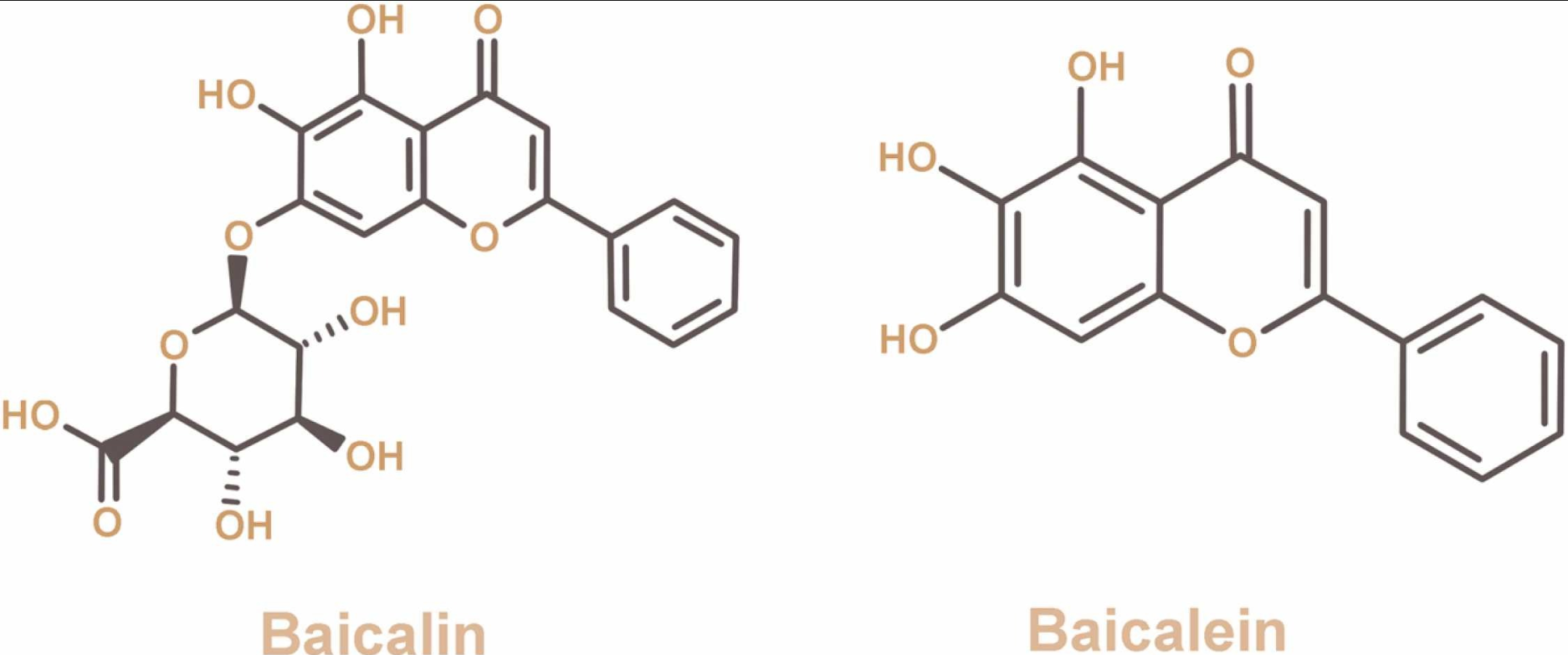
黄芩苷和黄芩素的化学结构:
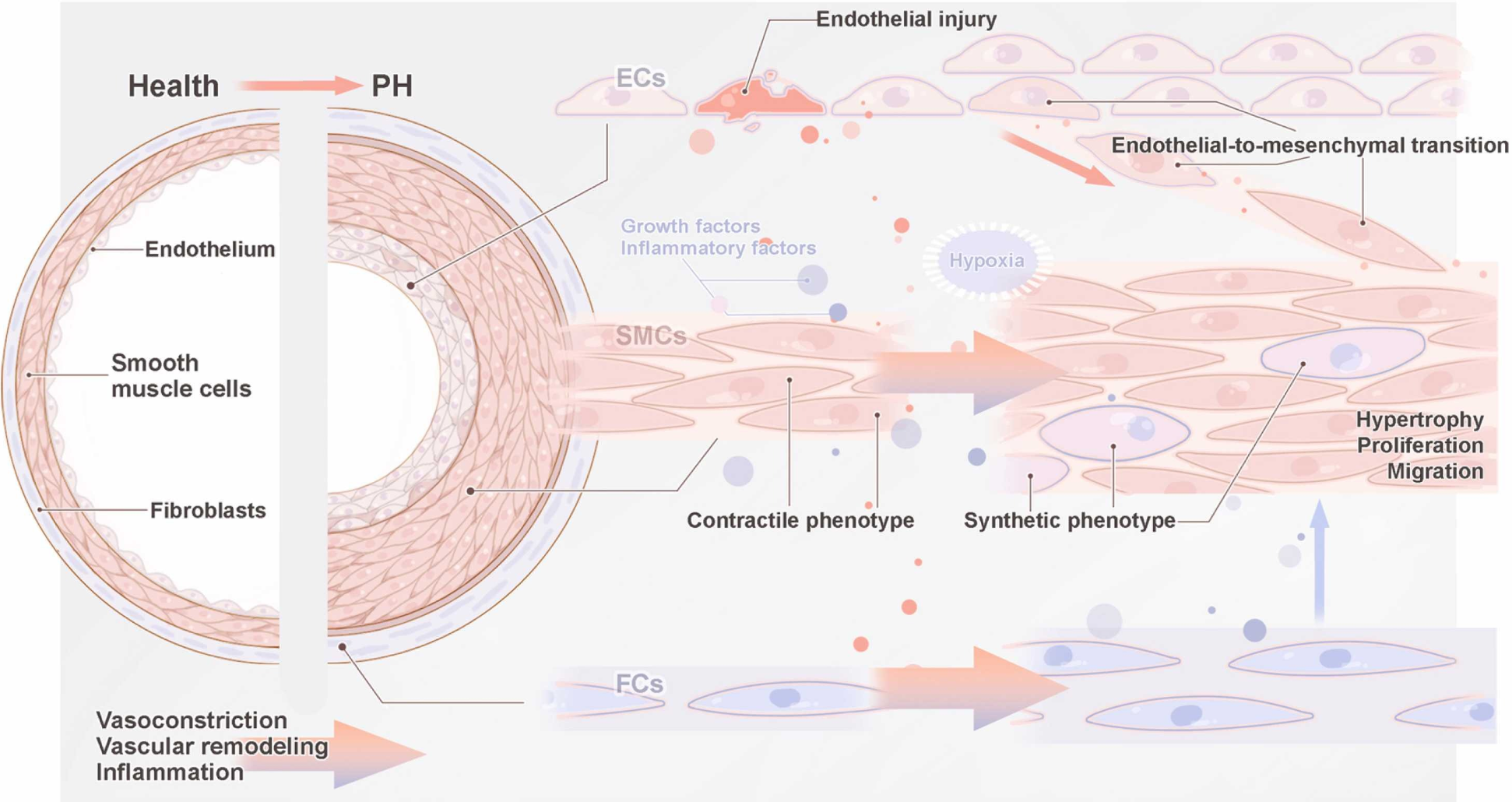
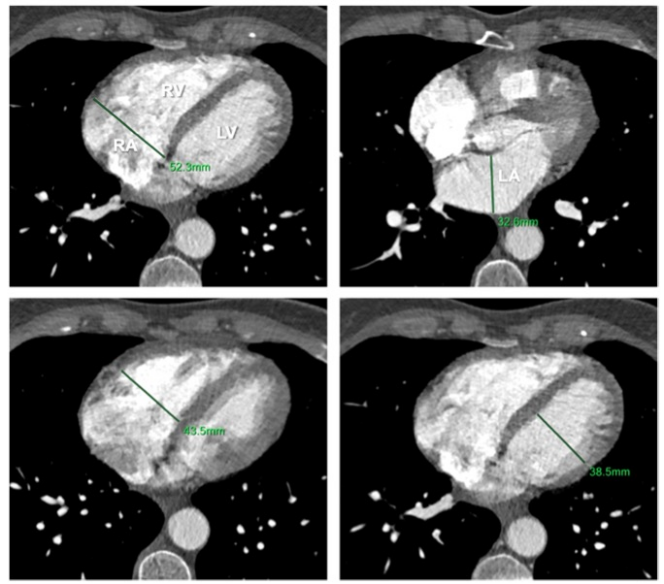
肺动脉高压血管重构的机制:
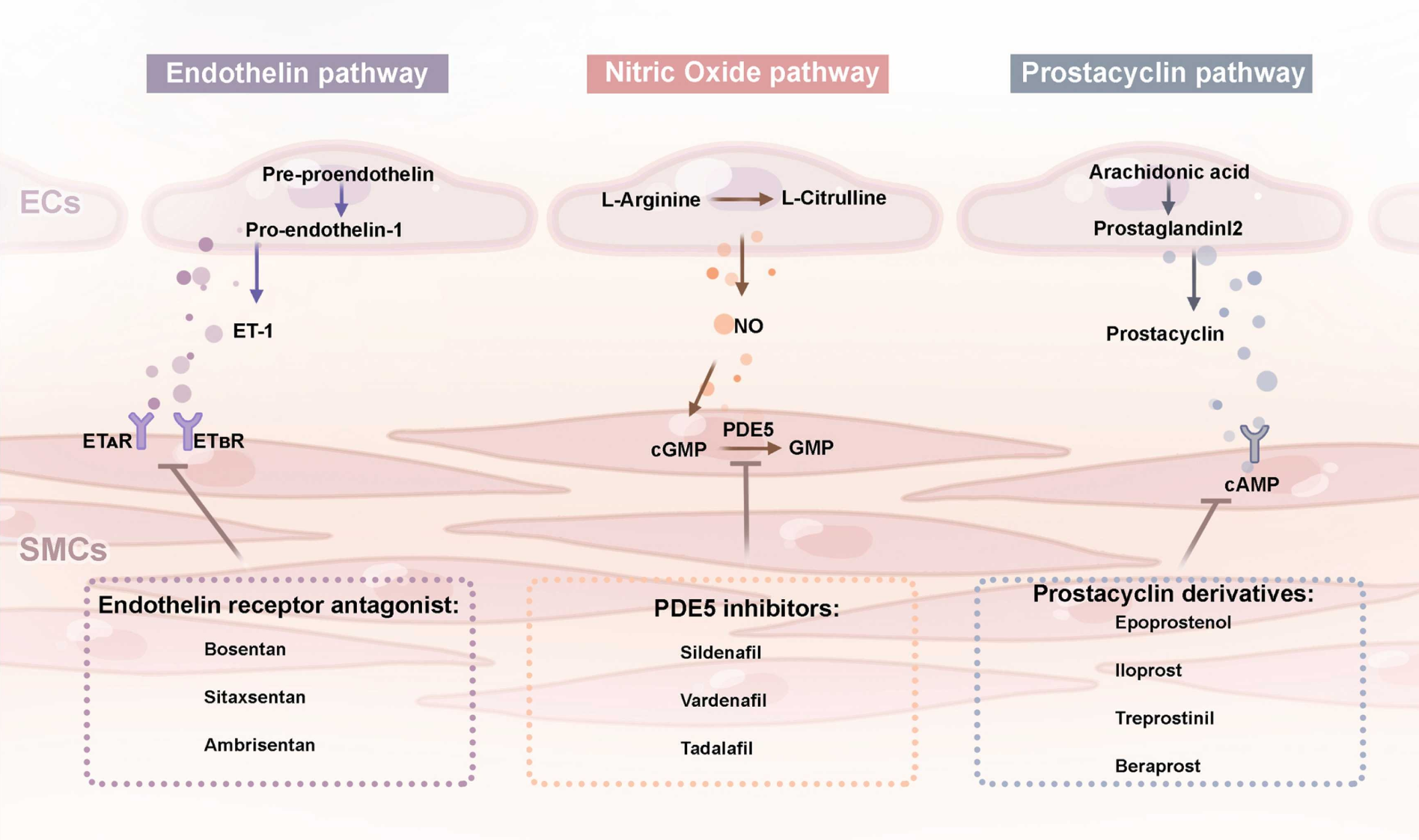
治疗PH的三种经典途径和代表性药物(主要包括内皮素途径、一氧化氮途径和前列环素途径):
黄芩苷和黄芩素对PASMCs和相关通路的影响:
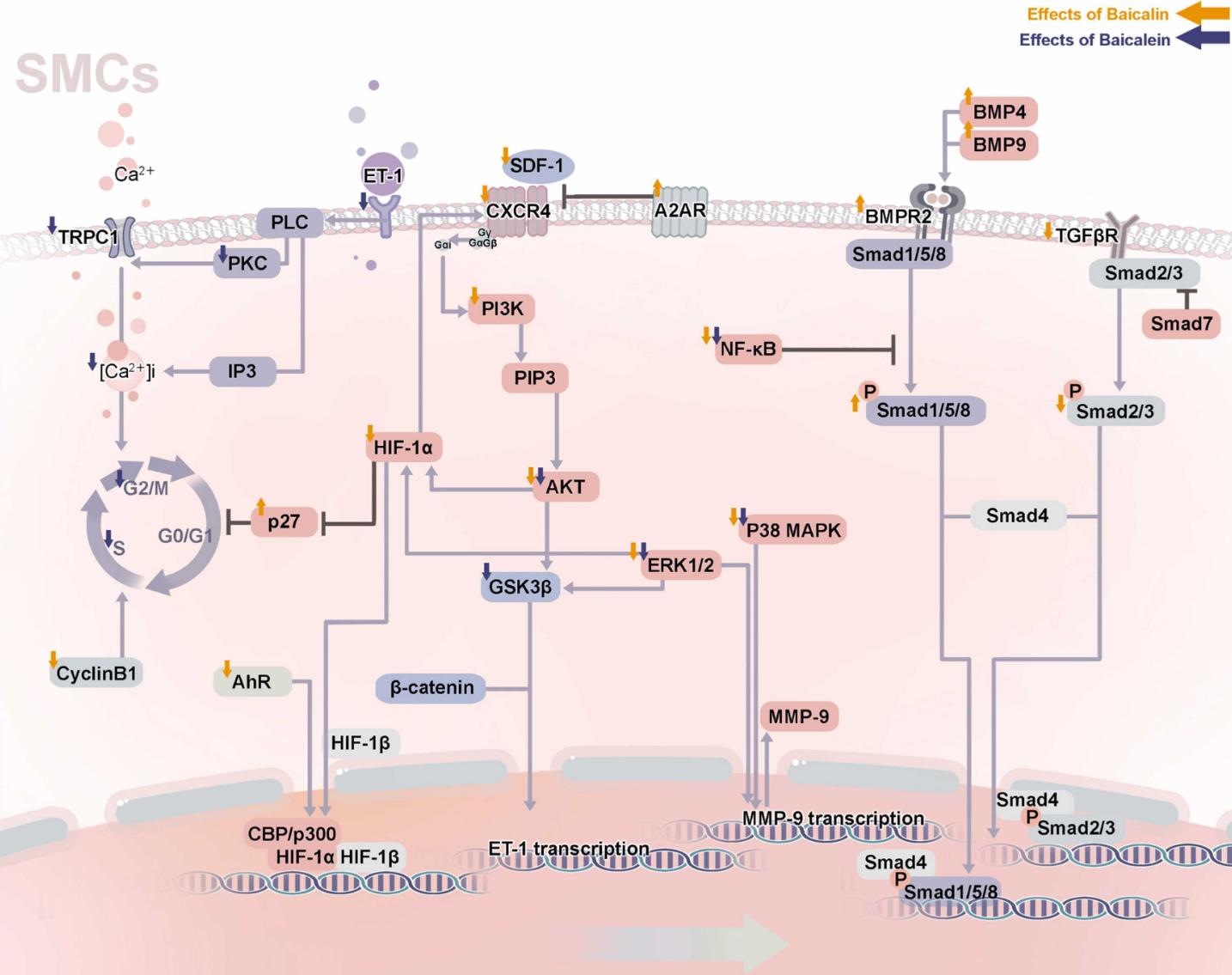
越来越多的证据表明,黄芩苷和黄芩素可通过抑制炎症、抑制 PASMCs 增殖、调节ECM 、减轻内皮损伤、预防 EndMT 和减轻氧化应激来有效预防和治疗 PH。尽管大量临床前试验证明了黄芩素和黄芩苷的积极作用,但它们的作用机制仍需进一步阐明。此外,大多数关于黄芩苷和黄芩素的研究都是在细胞水平或动物模型上进行的;它们的功效尚未在临床试验中得到证实。令人鼓舞的是,除了机理研究外,关于应用黄芩素和黄芩苷治疗 PH 的研究正在进行中。综上所述,黄芩苷和黄芩素对PH具有积极的预防和治疗作用,是预防和治疗PH的潜在有效药物。
原文:Cui L, Yuan T, Zeng Z, Liu D, Liu C, Guo J, Chen Y. Mechanistic and therapeutic perspectives of baicalin and baicalein on pulmonary hypertension: A comprehensive review. Biomed Pharmacother. 2022 Jul;151:113191. doi: 10.1016/j.biopha.2022.113191. Epub 2022 May 25. PMID: 35643068.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#Bio#
82
#动脉高压#
66
#黄芩苷#和#黄芩素#对#肺动脉高压#的作用机制和治疗前景,#黄芩#有一定的开发潜力,但是需要进行化学结构改造,以前改造的难度大,未来可以利用#人工智能#对其进行#药物设计#,应该有一定的潜力,有兴趣同学们可以试试
115
#Pharm#
74
#pharma#
67
#MAC#
78
中药的现代研究
63
#Med#
69