Rheumatology:尿蛋白可以预测活动性狼疮性肾炎和利妥昔单抗治疗的反应
2021-09-24 从医路漫漫 MedSci原创
约30%的系统性红斑狼疮(SLE)患者可能发展为狼疮性肾炎(LN)。LN的严重程度目前是通过肾活检来评估的,但血清或尿样中的生物标记物可能为非侵入性检查提供方法。
目的:约30%的系统性红斑狼疮(SLE)患者可能发展为狼疮性肾炎(LN)。LN的严重程度目前是通过肾活检来评估的,但血清或尿样中的生物标记物可能为非侵入性检查提供方法。williamhill asia 的目标是验证尿蛋白预测系统性红斑狼疮活动性肾损害的能力。
方法:收集197例系统性红斑狼疮患者和48例健康对照者的尿液标本。75例SLE患者有活动性LN,104例无活动性或非活动性肾脏疾病。利用MAGPIX Luminex平台,用MILLIPLEX®检测脂钙样前列腺素D合成酶(LPGDS)、转铁蛋白、α-1-酸性糖蛋白(AGP-1)、铜蓝蛋白、单核细胞趋化蛋白-1(MCP-1)和可溶性血管细胞粘附分子-1(SVCAM1)的含量。用二元Logistic回归分析蛋白质水平是否与肾脏活动性以及对利妥昔单抗治疗的反应有关。
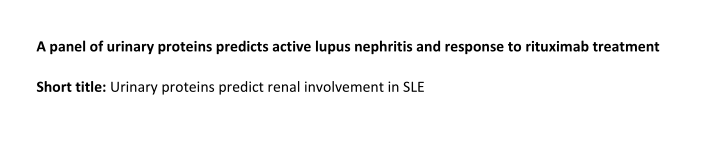
结果:系统性红斑狼疮患者尿转铁蛋白(P<0.005)、糖蛋白-1(P<0.0001)、单核细胞趋化蛋白-1(P<0.001)和可溶性血管细胞黏附分子-1(P<0.005)水平均显著高于正常对照组。SLE活动期LN患者血清转铁蛋白、AGP-1、铜蓝蛋白、单核细胞趋化蛋白-1和可溶性血管细胞黏附分子-1水平明显高于非活动期LN患者(P均<0.0001)。LPGDS、转铁蛋白、铜蓝蛋白、单核细胞趋化蛋白-1和可溶性血管细胞黏附分子-1 这5项尿蛋白的联合检测对活动期LN有较好的预测价值(AUC值为0.898)。LPGDS、转铁蛋白、AGP-1、铜蓝蛋白、单核细胞趋化蛋白-1和可溶性血管细胞黏附分子-1的联合模型预测了利妥昔单抗治疗12个月后的反应(AUC 0.818)。
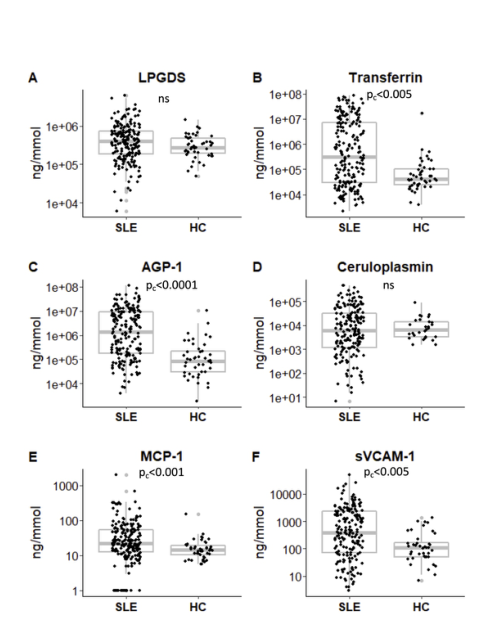
图1 系统性红斑狼疮患者与健康人尿蛋白水平的比较。SLE患者和正常人血清LPGDS(A)、转铁蛋白(B)、AGP-1(C)、铜蓝蛋白(D)、单核细胞趋化蛋白-1(E)和可溶性血管细胞黏附分子-1(F)的含量分析。方框图以灰色显示中值、IQR和极值,个别结果以黑点表示。采用Mann-Whitney U检验和Bonferroni调整来说明多重检测,以比较两组间尿蛋白水平的差异。报告了校正的P值(PC)。

图2 系统性红斑狼疮患者按疾病严重程度分组进行尿蛋白水平的比较。根据SLEDAI评分对SLE患者血清LPGDS(A)、转铁蛋白(B)、AGP-1(C)、铜蓝蛋白(D)、单核细胞趋化蛋白-1(E)、可溶性血管细胞黏附分子-1(F)和蛋白尿(G)进行分析。无-轻度被定义为0-4分,中等-5-14分,高度-非常高,15分及以上。方框图以灰色显示中值、IQR和极值,个别结果以黑点表示。采用Kruskal-Wallis检验和Dunn’s多重比较后检验比较两组间尿蛋白水平的差异。报告了校正的P值(PC)。
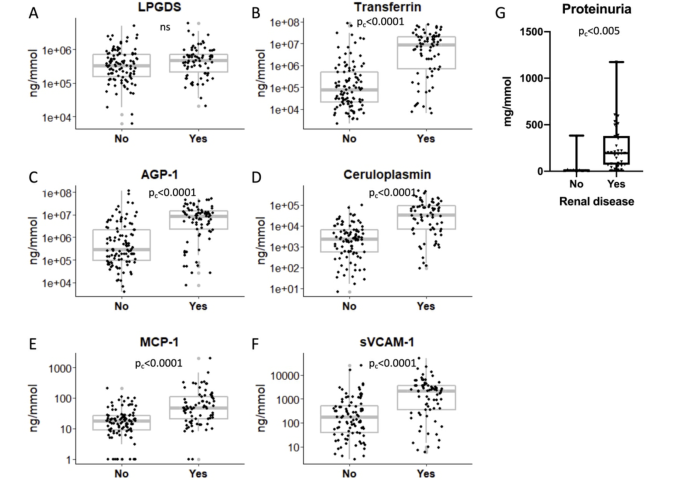
图3 系统性红斑狼疮活动性肾病患者尿蛋白水平的研究。系统性红斑狼疮患者血清LPGDS(A)、转铁蛋白(B)、AGP-1(C)、铜蓝蛋白(D)、单核细胞趋化蛋白-1(E)和可溶性血管细胞黏附分子-1(F)水平分析。方框图以灰色显示中值、IQR和极值,个别结果以黑点表示。采用Mann-Whitney U检验和Bonferroni调整来说明多重检测,以比较两组间尿蛋白水平的差异。报告了校正的P值(PC)。
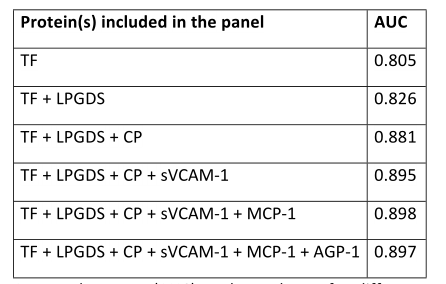
表1 将不同的蛋白质添加到回归模型显示曲线下面积(AUC)。TF:转铁蛋白,LPGDS:脂蛋白样前列腺素D合成酶,CP:铜蓝蛋白,sVCAM-1:可溶性血管细胞粘附分子-1,MCP-1:单核细胞趋化蛋白1,AGP-1: α -1-酸性糖蛋白。
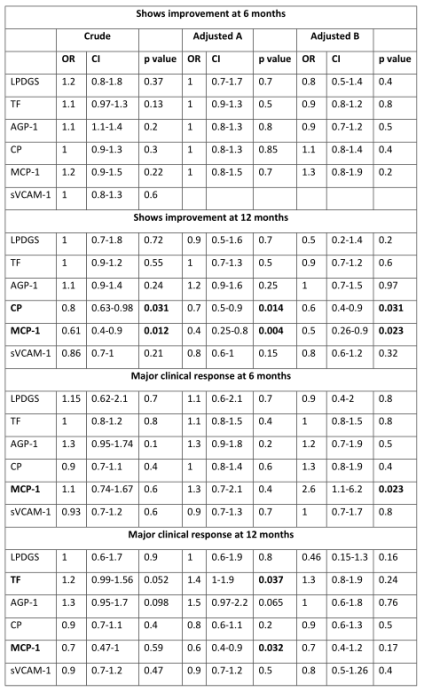
表2 尿蛋白预测利妥昔单抗治疗的反应;粗略的和调整后的优势比(OR),置信区间(CI)和p值显示了单独蛋白和联合利妥昔单抗治疗的反应。用于校正的模型包括混杂因素:年龄、病程、肾脏疾病和疾病活动性、抗dsdna抗体阳性、补体C3和/或C4低(模型A),或年龄、疾病病程、肾脏疾病和疾病活动性、口服类固醇剂量(模型B)。粗体标记的显著p值。
结论:研究结果支持在成人SLE患者尿蛋白提示活动性LN,并可以预测利妥昔单抗治疗的反应。需要进行前瞻性研究来证实研究结果。
原文出处
Davies JC, Carlsson E, Midgley A,et al,A panel of urinary proteins predicts active lupus nephritis and response to rituximab treatment.Rheumatology (Oxford) 2020 Dec 12
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#利妥昔#
64
#活动性#
77
#Rheumatology#
63
#尿蛋白#
64
#狼疮#
67
#肾炎#
54