Cancers:糖尿病与胰腺导管腺癌--患病率、临床病理变量和临床结局
2022-08-07 从医路漫漫 MedSci原创
胰腺导管腺癌(PDAC)是最常见的胰腺恶性肿瘤,占胰腺病变的90%以上。完全手术切除是治愈的唯一机会;然而,只有20%的患者被诊断为可切除的疾病。
背景:胰腺癌(PC)是全球癌症相关死亡的第七大原因。与其他恶性肿瘤不同,发病率持续上升,存活率略有提高。具体地说,胰腺导管腺癌(PDAC)是最常见的胰腺恶性肿瘤,占胰腺病变的90%以上。完全手术切除是治愈的唯一机会;然而,只有20%的患者被诊断为可切除的疾病。此外,80%的接受手术切除的PDAC在切除后五年内复发。PC患者的总5年生存率<5%。预后不良与几个因素有关,包括晚期诊断、早期远处转移、对大多数常规治疗方案的显著抵抗以及致密的肿瘤微环境。识别危险因素可能会导致胰腺癌的更早发现和更有利的预后。这种恶性肿瘤的一个潜在的重要危险因素是糖尿病(DM)。2型糖尿病(T2 DM)是最常见的糖尿病形式,估计约90%的糖尿病患者。高血糖是由于胰岛素抵抗和胰岛素分泌不足所致。临床和实验分析表明,胰腺癌经常与糖尿病的发病有关。研究证实,糖尿病确诊后的头两年内发生PDAC的风险最高。此外,外科手术,无论是惠普尔和远端切除,都可能导致新发糖尿病(NODM);然而,这种并发症的确切风险尚不清楚。NODM被定义为一种由胰腺内分泌实质丢失或破坏引起的疾病。
尽管DM和PDAC之间关系密切,但对T2 DM和NODM在PDAC中的确切患病率和对临床结局的影响知之甚少。关于这一主题的现有信息有限且前后不一致。各种研究表明,糖尿病对总存活率(OS)没有显著影响,而另一些研究发现,DM显著降低了存活率。
目的:本研究的目的是描述糖尿病在诊断为PDAC的患者中的患病率,分析DM的发生与临床病理因素的关系,并检测影响总体生存的变量。
方法:对病历资料进行回顾性分析。将患者分为非糖尿病组(n=101)和糖尿病组(n=74)。使用适当的检验进行了统计分析。
结果:DM组和NODM组患者的中位OS明显长于非DM组。结节受累、肿瘤部位、CEA、C反应蛋白和C反应蛋白/淋巴细胞比值与各型糖尿病患者的OS显著相关。在糖尿病组中,中性粒细胞减少的发生率较低。
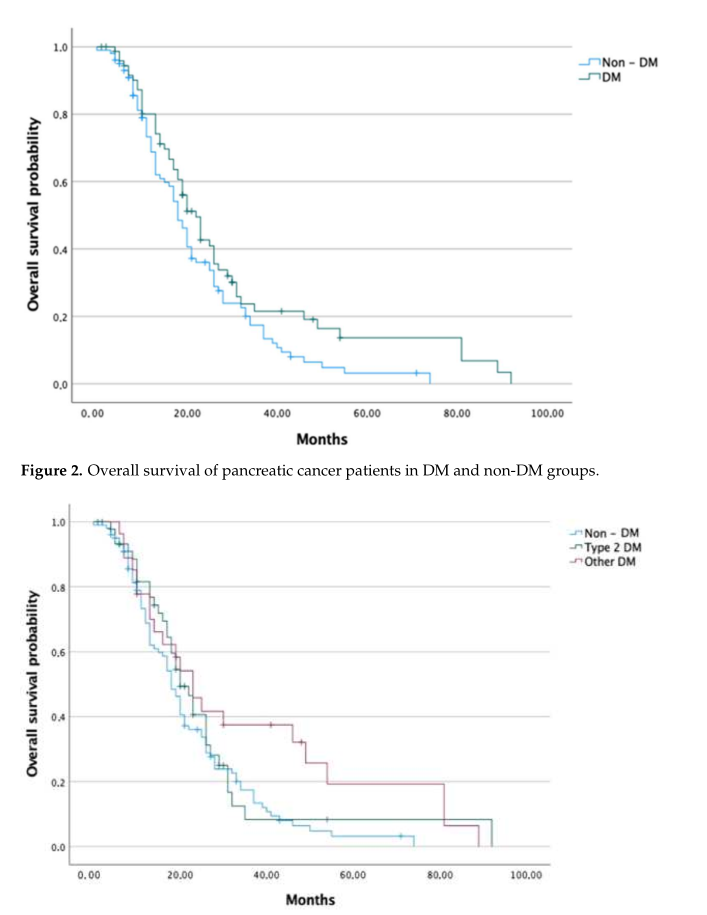
图1 非糖尿病、2型糖尿病和非糖尿病组中胰腺癌患者的总体生存率。
表1 总生存期--糖尿病组预后因素的单因素分析
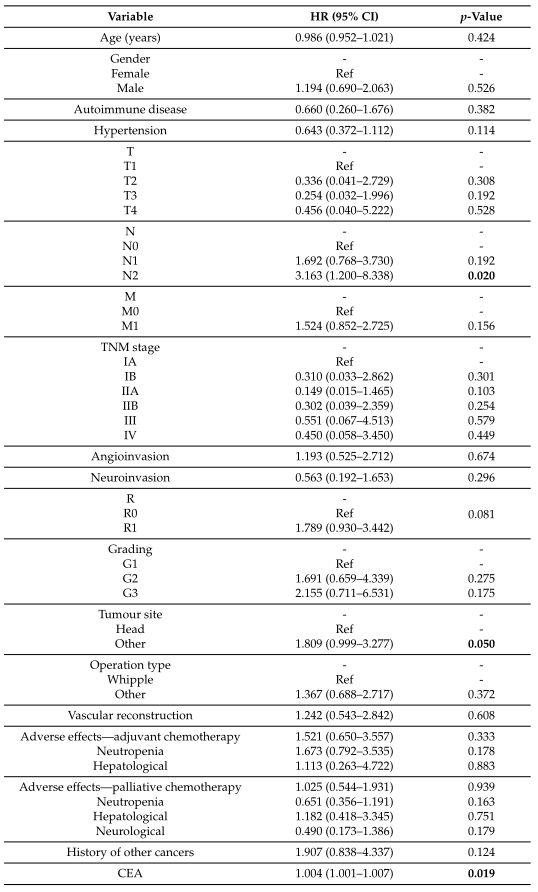
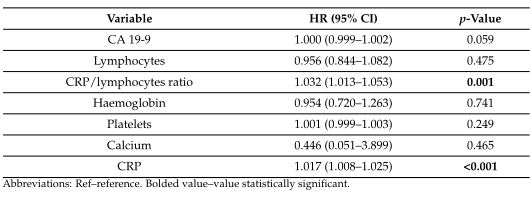
表2 影响总生存率的多因素分析--DM组。
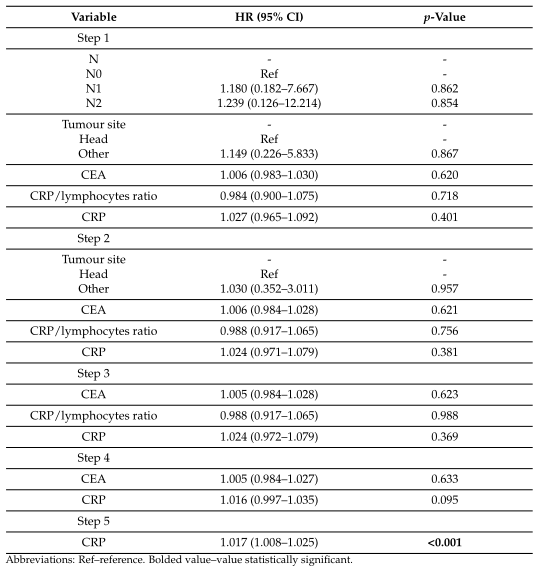
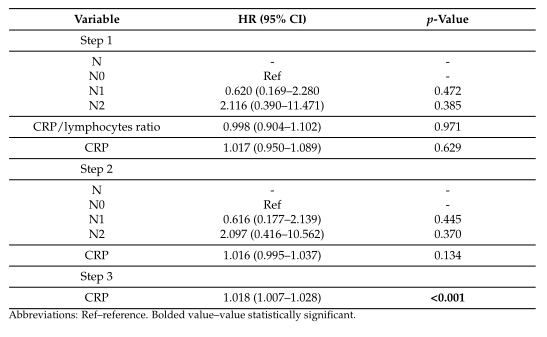
表3 总体生存预后因素的单因素分析--非糖尿病组。
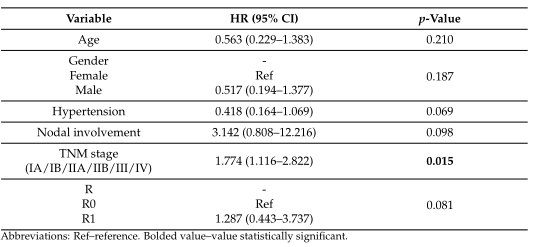
表4 影响总生存期的多因素分析--T2 DM组。
结论:糖尿病在胰腺癌患者中较为常见。在williamhill asia 的研究中,接受姑息化疗的糖尿病患者的中位OS显著高于未接受姑息化疗的患者。随着对糖尿病与胰腺癌关系机制的深入理解,需要进一步的研究,这可能会为新的预防和治疗策略的发展提供途径。
原文出处:Badowska-Kozakiewicz A, Fudalej M, Kwaśniewska D, et al.Diabetes Mellitus and Pancreatic Ductal Adenocarcinoma-Prevalence, Clinicopathological Variables, and Clinical Outcomes.Cancers (Basel) 2022 Jun 08;14(12)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#ERS#
119
#临床病理#
80
#临床结局#
61
#患病率#
68