European Radiology:用于预测头颈部鳞状细胞癌程序性死亡配体1表达的放射组学特征
2022-07-24 shaosai MedSci原创
最近,放射组学方法已被广泛用于肿瘤研究中。这些方法通过从这些数字生物医学图像中提取定量和高维数据,并反映细胞水平上的组织异质性潜力,可以在广泛获得的CT、MRI、PET和超声图像基础上提供信息。
 据统计,起源于口腔、咽部和喉部的头颈部鳞状细胞癌(HNSCC)占头颈部癌症的90%以上。近年来,免疫疗法在抗肿瘤治疗领域具有革命性意义。针对程序性死亡1(PD-1)/程序性死亡配体1(PD-L1)途径的免疫检查点抑制剂在HNSCC患者中显示出疗效和可控的安全性。PD-1主要在淋巴细胞和巨噬细胞中表达,而PD-L1是PD-1的配体。因此,在治疗前对HNSCC中PD-L1的表达进行准确的预测至关重要。检测PD-L1表达的一个常用方法是IHC。然而,IHC十分耗时且不能对PD-L1的表达进行实时评估。因此,寻找一种新的方法来预测PD-L1的表达在临床实践中至关重要。
据统计,起源于口腔、咽部和喉部的头颈部鳞状细胞癌(HNSCC)占头颈部癌症的90%以上。近年来,免疫疗法在抗肿瘤治疗领域具有革命性意义。针对程序性死亡1(PD-1)/程序性死亡配体1(PD-L1)途径的免疫检查点抑制剂在HNSCC患者中显示出疗效和可控的安全性。PD-1主要在淋巴细胞和巨噬细胞中表达,而PD-L1是PD-1的配体。因此,在治疗前对HNSCC中PD-L1的表达进行准确的预测至关重要。检测PD-L1表达的一个常用方法是IHC。然而,IHC十分耗时且不能对PD-L1的表达进行实时评估。因此,寻找一种新的方法来预测PD-L1的表达在临床实践中至关重要。
最近,放射组学方法已被广泛用于肿瘤研究中。这些方法通过从这些数字生物医学图像中提取定量和高维数据,并反映细胞水平上的组织异质性潜力,可以在广泛获得的CT、MRI、PET和超声图像基础上提供额外的有用信息。
近日,发表在European Radiology杂志的一项研究开发并验证了一种基于对比增强CT(CECT)的用于术前预测HNSCC的PD-L1表达的放射组学特征,为临床提供了一种新的预测PD-L1表达的无创影像学方法。
本研究共纳入了157名确诊的HNSCC患者,所有患者均接受了CECT扫描和肿瘤PD-L1表达的免疫组织化学检查。这些患者被分为训练集(n = 104;62个PD-L1阳性和42个PD-L1阴性)和外部验证集(n = 53;34个PD-L1阳性和19个PD-L1阴性)。从CECT图像中提取的放射组学特征构建了一个放射组学特征,并计算了一个放射组学分数。使用受试者操作特征分析评估了放射组学特征的性能。
最终选择了九个特征来构建放射组学特征。在训练和验证组中,放射组学特征区分PD-L1阳性和PD-L1阴性状态的性能良好,训练和验证组的受试者工作特征曲线下面积分别为0.852和0.802。

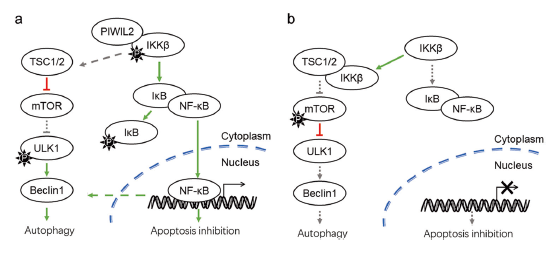
图 a 案例1:一名65岁男性的,患有鳞状细胞癌,PD-L1表达阳性。b 肿块的手动分割。c 免疫组化图像呈现PD-L1的阳性表达(×200;CPS=65)。放射性组学特征(A至I,见表2)的值分别为0.356、1.827、0.640、1.059、0.751、0.046、0.748、1.676和1.658。d 案例2:一名63岁男性,患有鳞状细胞癌,PD-L1表达阴性。e 肿块的手动分割。 f 免疫组化图像呈现PD-L1的阴性表达(×200;CPS<1)。放射学特征(A至I,见表2)的值分别为1.129、0.744、0.713、1.007、1.315、0.835、1.364、0.843和0.809。Rad-score为-2.203
本研究提出的基于CECT的放射组学特征模型在个体化评估HNSCC患者的PD-L1表达状态(CPS≥1与<1)方面表现良好,将有助于临床医生在治疗前对有望从抗PD-L1免疫疗法中获益的HNSCC患者进行筛选。
原文出处:
Ying-Mei Zheng,Ming-Gang Yuan,Rui-Qing Zhou,et al.A computed tomography-based radiomics signature for predicting expression of programmed death ligand 1 in head and neck squamous cell carcinoma.DOI:10.1007/s00330-022-08651-4
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#细胞癌#
79
#程序性死亡#
67
#PE#
67
#头颈部鳞状细胞癌#
82
#头颈部#
64
#颈部#
57