病例:食管裂孔疝,反流性食管炎
2019-08-29 王伯军 王伯军大夫谈消化
p.p1 {margin: 0.0px 0.0px 0.0px 0.0px; font: 11.0px 'Helvetica Neue'; color: #000000; -webkit-text-stroke: #000000; min-height: 12.0px} p.p2 {margin: 0.0px 0.0px 0.0px 0.0px; line-height:
病史
患者男性,40岁,进食后烧心,晚上宵夜后立刻睡觉有食物反流现象,既往黑便史。
过去身体健康情况一般,无特殊疾病,幼年有哮喘。
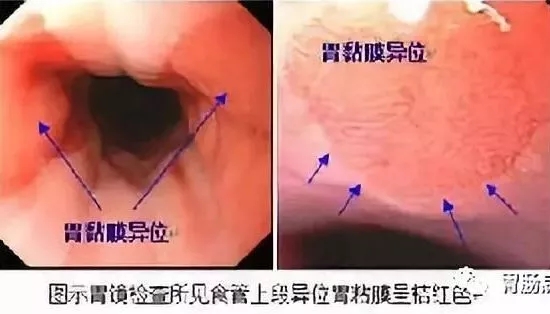
胃镜:1. 反流性食管炎D级;2. 食管裂孔疝?3. 慢性非萎缩性胃炎伴糜烂。
该如何治疗?
分析
根据患者症状结合胃镜检查,可明确诊断:反流性食管炎。
反流性食管炎的主要原因是:食管下括约肌松驰,使胃酸反流进入食管;食管体部运动异常,使食管清除胃酸时间延长等;其他有食管外诸多机械因素,如食管裂孔疝、胃排空延迟等等。
根据患者胃镜检查情况,患者反流性食管炎的主要原因是食管裂孔疝。
胸腔与腹腔之间有一个分隔,叫横膈,其上有一个孔,叫食管裂孔,食管通过这个孔与胃连接,当食管裂孔扩大时,胃的一部分就会通过这个孔进入胸腔,这就是食管裂孔疝。其主要原因是食管发育不全、食管裂孔部位结构削弱。
食管裂孔疝形成以后,使食管与胃之间的隔角发生改变,很容易发生胃食管反流。
食管裂孔疝的诊断,胃镜检查只能提示难以确诊,确诊需要X线胃食管造影检查。
反流物主要是胃酸,还可能有胆汁、胰液等。由于经常反流,反流物对食管黏膜产生慢性损伤,从而发生食管充血、水肿、糜烂、甚至溃疡,这就是反流性食管炎。其主要症状为反酸、烧心。
进食能促进胃酸分泌,胃酸反流致食管就发生烧心。夜间迷走神经兴奋性增高,本来胃酸分泌就增多;平卧状态失去了重力向下作用;夜间睡眠期间又少了唾液对食管的冲洗,因此夜间酸反流对食管刺激损伤更大,饱食后睡觉对食管伤害更甚。
反流性食管炎依病变严重程度可分为A、B、C、D四级,D级是最严重的,依患者的胃镜检查报告单及图片来看,患者的食管炎属于D级,这是最严重的食管炎。且患者有黑便史,这说明曾发生过消化道出血,而根据患者胃镜表现,患者的食管糜烂很可能会发生出血。
食管炎除了反酸、烧心这些症状外,还可以发生食管狭窄、易并发食管癌,尤其是重度食管炎,必须予以重视。
治疗建议
1. 艾司奥美拉唑片20mg早、晚饭前半小时口服每日2次,莫沙比利片5mg每日3次饭前半小时口服,尿囊素铝片2粒每日3次饭前半小时,以抑酸、促进食管胃的蠕动、促进食管炎症糜烂修复。
以上药物可治疗2个多月,复查胃镜观察食管糜烂愈合的情况。
由于患者食管糜烂特别严重,建议患者可以再开始一个月加用中成药,促进食管糜烂、溃疡处肉芽组织的生长,促进病变局部新生血管的形成,从而有利于糜烂溃疡愈合。
患者食管炎主要由食管裂孔疝引起,而食管裂孔疝一旦形成,解剖结构发生改变,目前没有药物能纠正。目前的药物只能控制症状、修复食管局部炎症糜烂,不能解决引起食管炎的根本问题。鉴于患者的情况,即使3个月以后复查胃镜食管糜烂、溃疡已经愈合,一旦停药仍会出现反酸、烧心,时间一长又会引起食管损伤,因此,患者很可能需要长期服药,建议患者3个月后复查胃镜。若食管糜烂愈合,仍用小剂量药物维持治疗,如雷贝拉唑片10mg早饭前半小时口服,以控制反酸、烧心等症状。其后每1~2年进行一次胃镜复查。
2. 调整饮食,改变生活方式,可以减少胃食管反流,这是治疗胃食管反流病的基础。
1)避免以下食物,可减轻胃食管反流。
高脂肪食物、酸及甜的食物、柑橘类水果、西红柿、辣椒、生大蒜及洋葱、巧克力、咖啡因、烟酒。
要多摄取含有膳食纤维的蔬菜,这可减轻胃食管反流。
2)改变生活方式,以减轻反流症状。
进食八分饱,汤水少喝要分次喝;餐后要有30分钟活动时间,不要做弯腰动作;睡前3小时不吃东西;床头抬高至少15cm,注意是抬高床头的床脚,使床板呈床头处高床脚处低,15度倾斜;控制体重,避免肥胖。
夜间酸反流对食管损伤更严重,睡前3小时绝对禁止进食,否则会促进夜间胃酸分泌,加重胃食管反流。
3. 患者年纪尚轻,若在调整饮食、改变生活方式后反酸烧心仍然很明显,需要大剂量质子泵抑制剂来控制症状,则建议患者进行手术治疗。
患者发生食管癌的几率较小,大多能用药物来控制,待这次食管炎愈合后,用最小剂量的质子泵抑制剂,如雷贝拉唑10mg/d或奥美拉唑10mg/d来控制酸反流,关键是控制症状,症状得以控制则可防止食管炎再发,1~2年复查一次胃镜观察食管情况。平时需注意饮食和生活方式的改变。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#食管裂孔疝#
73
#食管#
42
#食管炎#
51
#疝#
57
#反流#
62