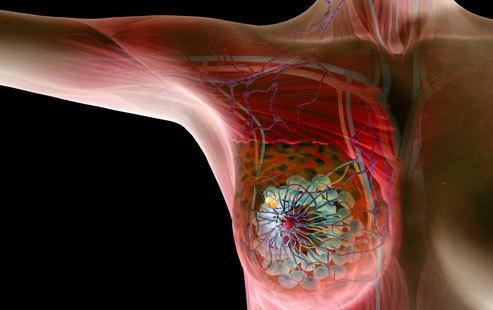
Clini Cancer Res:PD-L1表达与三阴性乳腺癌新辅助化疗预后的相关性
2020-07-26 MedSci原创 MedSci原创
既往研究表明三阴性乳腺癌患者可从PD-1轴免疫疗法中获益。因此,本研究评估PD-L1在肿瘤细胞和免疫细胞上的表达与TNBC患者采用新辅助度伐单抗联合化疗获益的相关性。
在转移背景下的IMpassion 130试验和新辅助化疗背景下的Keynote 522试验中,三阴性乳腺癌(TNBC)患者均从PD-1轴免疫疗法中获益。因此,本研究拟采用定量免疫组化方法来检测PD-L1在肿瘤细胞和免疫细胞上的表达,以评估PD-L1表达与TNBC患者采用新辅助度伐单抗联合化疗获益的相关性。
方法:
获取参与I/II期临床试验(NCT02489448)的患者的治疗前针刺活检组织(n=69),根据组织质量,最终分析纳入了45位患者(qCR=18、非-pCR=27)。
结果:
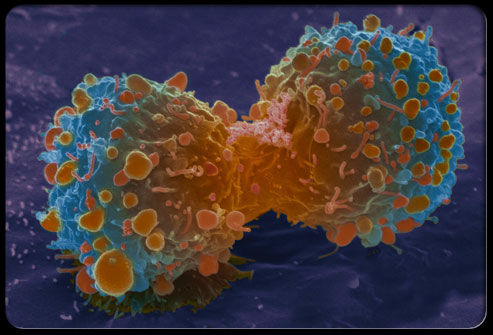
与非-pCR患者相比,pCR患者肿瘤细胞、CD58阳性细胞和基质上PD-L1的表达明显升高。在pCR和非pCR病例中,肿瘤或间质间室中CD68阳性细胞的数量没有差异
结论:
PD-L1在肿瘤细胞、间质免疫细胞中表达,并与CD68阳性细胞共定位,与TNBC患者采用度伐单抗联合化疗治疗的高pCR率相关。
原始出处:
Fahad Shabbir Ahmed,et al. PD-L1 protein expression on both tumor cells and macrophages are associated with response to neoadjuvant durvalumab in triple negative breast cancer (TNBC). Clinical Cancer Research. July,2020. DOI: 10.1158/1078-0432.CCR-20-1303
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#新辅助#
36
#阴性乳腺癌#
49
#相关性#
36
#PD-L1表达#
40
#PD-L1#
40
#三阴性#
31