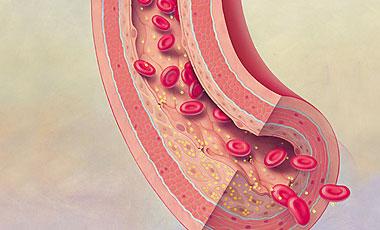
Eur Heart J:他汀类药物可预防静脉血栓
2017-03-29 MedSci MedSci原创
莱斯特大学和布里斯托尔大学的研究人员已经发现进一步的证据表明,他汀类药物可以“显著降低”身体某些部位血液凝固的发生。
莱斯特大学和布里斯托尔大学的研究人员已经发现进一步的证据表明,他汀类药物可以"显着降低"身体某些部位凝血的发生。
研究团队对几项降低胆固醇的药物研究进行了分析,发现该类药可能在降低静脉血栓栓塞(VTE)的复发风险中起潜在作用。
该研究获得东米德兰健康应用研究与护理中心的NIHR项目的资助,结果发表在《European Heart Journal》上。
最新研究结果与同组1月发表的研究报告类似,该研究小组建议他汀类药物能将病情的威胁降低15%至25%。
谈到最新的研究,该研究参与人,莱斯特大学初级保健糖尿病与血管医学教授,NIHR CLAHRC East Midlands院长,莱斯特糖尿病中心联合主任Kamlesh Khunti教授说,"曾经有迹象表明他汀类药物可能在预防VTE方面发挥潜在作用,但证据不足。"
"williamhill asia
想进一步探讨这个问题,将所有研究结合起来,以评估他汀类药物与复发性VTE之间的关系。尽可能多的了解这种情况对williamhill asia
来说很重要,因为据说世界上每6秒就会有一个人死于VTE。"
"尽管严重,但是只要得到正确的照顾,绝大多数血块是可以完全避免的。然而,治疗为英国的卫生服务带来相当大的经济负担,因为它被认为需花费大约6.4亿英镑来管理病情。"
在此过程中,对基于他汀类药物和VTE 的8项研究进行了汇总分析,其中涉及到103,500多名参与者。
来自布里斯托尔大学临床科学学院肌肉骨骼研究组的首席研究员Setor Kunutsor博士说:"虽然williamhill asia
的研究还没有发现VTE的原因,但是在处理这种病症时,利用他汀类药物治疗确实具有潜在作用。"
"williamhill asia
的研究显示,大量的证据表明,他汀类药物可能在VTE的一级和二级预防中起着潜在的作用。"
希望这一发现可以产生新的指导方针和扩大其在心血管疾病预防中的使用。
原文出处:
本文系williamhill asia 医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#静脉血#
57
#他汀类药#
43
#静脉#
43
#ART#
0
#HEART#
0