Blood:PD-1抗体pembrolizumab治疗慢性淋巴细胞白血病Richter’s转化有效
2017-04-25 任我行@血液科 肿瘤威廉亚洲官网
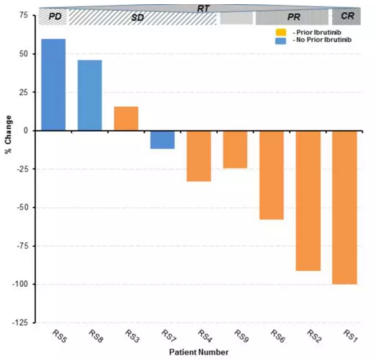
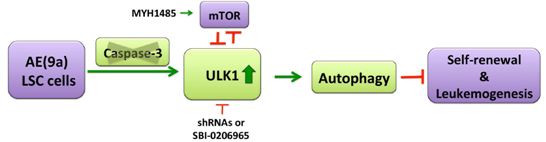
慢性淋巴细胞白血病(CLL)Richter’s转化,是指CLL患者继发侵袭性淋巴瘤(绝大部分为弥漫大B细胞淋巴瘤[DLBCL],小部分为霍奇金淋巴瘤)。Richter’s转化的患者预后极差,目前缺乏有效的治疗,异基因造血干细胞移植有可能改善一部分年轻患者的预后。在最新一期Blood中,Ding Wei等发布了PD-1抑制剂治疗Richter’s转化的结果,有望为这一高度侵袭性疾病的治疗带来希望
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#mAb#
48
#淋巴细胞白血病#
37
#Pembro#
58
#PE#
35
#Pembrolizumab#
51
#淋巴细胞#
30
#ICH#
36
#PD-1抗体#
34